What happens if you need medical care in a hospital, but you are not already registered as a patient?
Sometimes nothing.
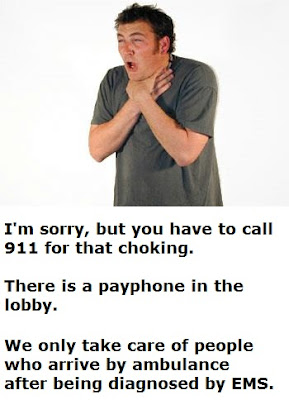
This is what should have happened.
–
–
When Wallace fell and broke her hip earlier this month in the lobby of the Greater Niagara General Hospital, she assumed she would be quickly taken care of, but that was not the case, according to the Toronto Star.
Instead, she was told to call an ambulance.[1]
In the US, EMTALA (Emergency Treatment and Active Labor Act)[2] states that anyone within 250 of the hospital entrance must be assessed and stabilized prior to any transfer or discharge. So, this should not happen, but this was not in the US.
How well that works for patients in the US is a different story. I have taught ACLS[3] in several hospitals and has members of a few of the hospitals’ rapid response teams tell me that they have been ordered not to treat anyone who does not have a patient identification bracelet on. I didn’t believe this was true, so I checked sand had this confirmed by my boss at one hospital.
This apparently comes from the lawyers. What part of EMTALA don’t they understand?
What part of public relations don’t they understand.
Whatever the rules are, your best defense in court is to do what is best for the patient. If you don’t know what you are doing, let somebody else do something. How do the hospital personnel leave a patient on the ground and pretend that they are in any way behaving ethically?
–
–
“I was disappointed this week to learn of a situation where a family did not receive the standard of care they deserved after their mother fell in the entrance area of our Niagara Falls site,” Niagara Health System Supervisor Dr. Kevin Smith wrote in a statement.[1]
It is a start, but the problem is not that a family did not receive the standard of care. The problem is that a hospital has rules that discourage their doctors, nurses, and everyone else from taking care of people.
The problem was not that they did not treat the family when the mother fell. The problem is that they did not treat the mother who fell.
We can be sued for anything. Frivolous lawsuits are supposed to be thrown out by a judge, when the judge is reviewing the case to determine if it has any justification.
Not treating injured people in a hospital is just asking to be sued.
–
“In response to this latest incident, and to ensure clarity to all members of our health care team, I have conveyed to NHS leadership that our policy for response to any visitor in distress will be to ensure a rapid response and transport to the most appropriate clinical setting,” Smith wrote.[1]
Why does this require a special announcement?
Why is this not a part of day one of orientation?
–
Footnotes:
–
[1] Elderly Woman Injured in Hospital Told to Call Ambulance
By Christina Ng
ABCNews.go.com
Oct 20, 2011 11:53am
Article
–
[2] EMTALA
EMTALA.com
Web page
#2 from the FAQ page –
Any patient who “comes to the emergency department” requesting “examination or treatment for a medical condition” must be provided with “an appropriate medical screening examination” to determine if he is suffering from an “emergency medical condition”. If he is, then the hospital is obligated to either provide him with treatment until he is stable or to transfer him to another hospital in conformance with the statute’s directives.
What constitutes “coming to the emergency department”? See our special note on the 250 yard rule and its discussion of presentations to locations other than the emergency room, as well as the further discussion below.
If the patient does not have an “emergency medical condition”, the statute imposes no further obligation on the hospital.
–
[3] Advanced Cardiac Life Support
Basically CPR with some drugs thrown in to make the doctors, nurses, and medics feel as if they are better than those without these drugs. CPR = CardioPulmonary Resuscitation –
1. Call for help and confirm unresponsiveness.
2. Place your hands on the center of the sternum and Push Hard and Push Fast.
3. Repeat until a defibrillator is available, continue compressions while attaching the defibrillator, shock if indicated, and resume until something changes.
.


We actually had this exact discussion during ethics class the other night, and I was shocked to find that that is the policy of our local hospital as well, and I AM in the US. When asked about EMTALA and the responsibilities it imposed our instructor responded with “that’s a good point – I’ll have to bring that up to the board”
Seriously ?!?
It is sad that lawyers and bureaucrats are now the people responsible for setting the standard of care in our hospitals.
Interesting. Long, long ago, on a naval base far, far away (well, Maryland), I was dispatched for a CPR in progress in the hospital parking garage. As we approached the scene, the hospital code team arrived. Never have I seen such chaos. We identified the physician nominally in charge, verified that our services would be superfluous, and took our leave. That incident made me think that if I ever found myself in similar circumstances, I would *prefer* that someone call 911.
Fast forward ~15 years…I had the unusual and unfortunate circumstance to be in just this position…a non-patient in a hospital who suddenly needed medical assistance (due to a slip-and-fall in the lobby which refracted my previously-injured-but-allegeldy-healed right tibia). There was a quick response from a designated team in the ED, I was assisted onto a stretcher, and got VIP service from the ED (in and out of a level I trauma center ED in under 3 hours on a Friday afternoon/evening, with X-rays and splinting). My experience locally is that every hospital has such a setup.
So maybe things aren’t the same all across the country. Or maybe we’re unusually lucky out here in the wild west.
I find this amazing!
I’m only a First Aider (and a once and will be again volunteer with the Ambulance Service) in the UK, but I would expect to treat any patient presented to me if I thought I could help.
Medical and Nursing professionals here could run the risk of being struck off if they did not give treatment – albeit sometimes emergency treatment only – to a patient who needed it urgently.
I can understand the (slightly perverse) logic that, where a hospital is run for profit, only potential paying customers or those who have the proof that someone else will pay will get treatment. Notwithstanding that, don’t medics have any form of Hippocratic responsibility – or do they now take the “hypocritical” oath?
The only reason, IMHO, for refusing to treat is if treatment is likely to result in the practitioner’s injury or death – not that they won’t get paid.
Frankly, I’m disgusted.
A similar incident happened a few months ago, I think in Portland, where an ambulance was called to a cardiac arrest in a hospital parking garage.
I once responded, lights and sirens, to a hospital’s parking lot for a patient who had a panic attack after getting discharge. We were called by hospital security, who said they could not driver her around the parking lot in their car. Apparently they thought the risk of doing so was more than us crashing on the way there.
Perhaps I should mark 250 feet from the hospital entrance.
Vexatious litigants once again manufacture chaos and fear, where sanity and care ought to prevail.