.jpg)
Also posted over at Paramedicine 101 (now at EMS Blogs) and at Research Blogging. Go check out the excellent material at these sites.
–
Is it safe to treat CHF/ADHF (Congestive Heart Failure/Acute Decompensated Heart Failure) with IV (IntraVenous) bolus doses of NTG (NiTroGlycerin or GTN – GlycerylTriNitrate in Commonwealth countries)?
Well, it isn’t too dangerous to study.
–
all patients received an initial 2-mg intravenous bolus of highdose nitroglycerin, . . . Subsequent 2-mg boluses of high-dose nitroglycerin were permitted every 3 to 5 minutes at the discretion of the treating emergency physician. Repeated administration of high-dose nitroglycerin was allowed for a period of up to 30 minutes, resulting in a maximum potential dose of 20 mg (2 mg every 3 minutes for 30 minutes).[1]
Those high doses are enough to give a stroke to the doctors, nurses, and medics who think that CHF = Lasix (furosemide), but I am not writing this for people stuck in the 1980s. Most doctors, nurses, and medics appear to realize that nitrates are the most effective medication for CHF. The important question is How aggressive is too aggressive?
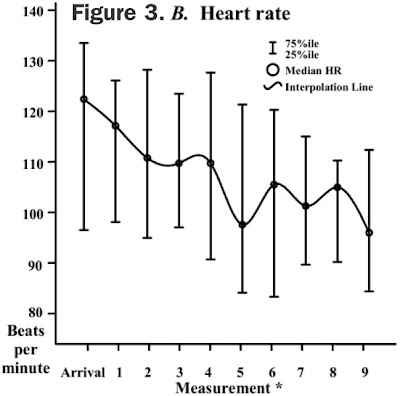
What was the effect on heart rate? We want to avoid bradycardia, which is a side effect of too much NTG.
–
–
Bradycardia does not seem to be a problem. As with severe pain, there is so much excess that a decrease does not even bring rates down into the normal range.
–
–
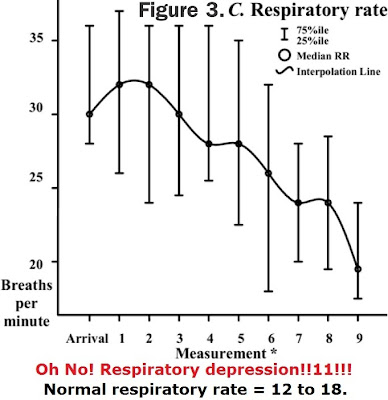
With respirations, the high dose NTG also only drops the rate to around the upper end of normal. Not exactly the life threat that nitrate alarmists pretend will occur.
–
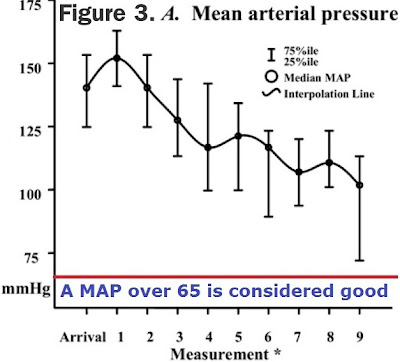
We can’t skip blood pressure. This is the terror for those opposed to high doses of nitrates.
What about the hypotension?
If the blood pressure drops, it will stay that way – forever.
If you keep making that face, it will stay that way – forever.
Everybody knows that high doses of NTG will bottom out the blood pressure.
–
–
High doses of NTG only rarely cause a significant drop in blood pressure and that resolves spontaneously – just as it does with standard doses of NTG. These patients remained hypertensive, but with their blood pressures much less dangerously elevated than before the high dose IV boluses of NTG.
–
Maybe they did not give much NTG.
The majority (34.5%) of patients received 3 boluses of high-dose nitroglycerin (Figure 2), and the mean dose of high-dose nitroglycerin administered was 6.5 mg (95% CI 5.2 to 7.8 mg).[1]
Following the protocol, the doses could have been much higher, but they are reassessing patients prior to giving further doses.
–
Wouldn’t patients receiving standard doses of NTG by pump would receive similar total doses?
20 μg/minute – 40 μg/minute would receive 0.6 mg – 1.2 mg (600 μg – 1,200 μg) over half an hour (the duration of the experimental dosing). Is there a difference between less than 1 mg and over 6 mg?
–
I left out one other bit of information. These patients were not just receiving bolus NTG. They were receiving the boluses in addition to IV NTG by pump.
The mean initial and final intravenous nitroglycerin infusion rates were 23.6 μ g⁄minute (95% CI 15.4 to 31.9 μ g⁄minute) and 50.2 (95% CI 37.9 to 62.5 μ g/minute) for patients who received high-dose nitroglycerin. The mean initial intravenous nitroglycerin infusion rate for the nonintervention group was 31.7 μ g⁄minute (95% CI 26.0 to 37.3 μ g⁄minute); the final intravenous nitroglycerin rate for nonintervention patients was not available.[1]
The infusion rate for IV NTG started out within the range I gave, but ended up higher than that range, while they were receiving high dose boluses of IV NTG.
Not only are high dose boluses of IV NTG not the instant hypotension/death that some would have us believe, but they can be added to moderate dosing of IV NTG infusions and still not cause problems.
–
But what were the results?
First the baseline conditions –
–

Click on the images to make them larger.
–
I point out that the patients being treated with high dose boluses of IV NTG were much sicker starting out, but I have not shown the improvement.
The primary effectiveness endpoint of endotracheal intubation within 6 hours occurred in 13.8% (95% CI 4.8% to 29.5%) of patients treated with high-dose nitroglycerin and 26.7% (95% CI 15.5% to 40.8%) of the nonintervention patients.[1]
With high dose IV boluses of NTG 13.8% of patients were intubated.
Without high dose IV boluses of NTG 26.7% of patients were intubated.
High dose IV boluses of NTG cut the intubation rate almost in half.
–
The primary safety endpoint of cardiovascular complications was 20.7% (95% CI 9.1% to 37.8%) in the high-dose nitroglycerin group (17.2% [95% CI 6.9% to 33.7%] with myocardial infarction and 3.5% [95% CI 0.4% to 15.0%] with symptomatic hypotension) and 28.9% (95% CI 17.3% to 43.1%) of the nonintervention patients (all due to myocardial infarction, with no episodes of symptomatic hypotension).[1]
With high dose IV boluses of NTG 20.7% of patients had cardiovascular complications –
17.2% had heart attacks.
3.5% had symptomatic hypotension.
Without high dose IV boluses of NTG 28.9% of patients had cardiovascular complications
28.9% had heart attacks.
Zero% had symptomatic hypotension.
–
By golly, the warnings about hypotension were right!
the occurrence of symptomatic hypotension in the high-dose nitroglycerin group corresponded to a single instance that developed after administration of one 2-mg dose and resolved with a 500-mL fluid bolus, without evidence of further complications.[1]
As I have stated elsewhere,[2],[3] the 500 ml fluid bolus probably was not necessary, since nitrate-induced hypotension resolves spontaneously and without complications.
–
A rapid and profound decrease in blood pressure was also observed with use of high-dose nitroglycerin, without an associated increase in adverse events. Though encouraging, these results are preliminary, and the next logical step in the evaluation of high-dose nitroglycerin is an adequately powered, multicenter, prospective, randomized, double-blind, comparison trial. According to our investigation, conduction of such a trial seems feasible.[1]
I keep hearing excuses for why this study is too dangerous to study.
A better conclusion is that it is too dangerous to not study.
Where is the evidence of danger?
Heart failure is one of the five most common admitting diagnoses in the US, so how can we ignore this? More than heart attack. More than asthma. More than almost everything else.
–
–
Footnotes:
–
[1] Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis.
Levy P, Compton S, Welch R, Delgado G, Jennett A, Penugonda N, Dunne R, Zalenski R.
Ann Emerg Med. 2007 Aug;50(2):144-52. Epub 2007 May 23.
PMID: 17509731 [PubMed – indexed for MEDLINE]
Free Full Text PDF Download from Ferne.org
–
[2] Is IV NTG Too Dangerous for EMS
Rogue Medic
Article
–
[3] EMS NTG for CHF – Bolus or Infusion – Part II
Rogue Medic
Article
–
Levy P, Compton S, Welch R, Delgado G, Jennett A, Penugonda N, Dunne R, & Zalenski R (2007). Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Annals of emergency medicine, 50 (2), 144-52 PMID: 17509731
.



[…] posted over at Rogue Medic (now at EMS […]