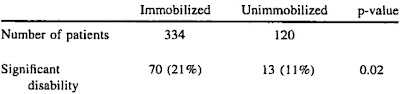
Another comment on How Much Harm Does Spinal Immobilization Cause demonstrates the horribly flawed logic that is applied by defenders of alternative medicine and other forms of bad medicine. This post was describing the doubling of disability among patients with unstable spinal fractures treated with spinal immobilization, when compared with those not treated with spinal immobilization. SCI is Spinal Cord Injury.
Anonymous writes –
Can I suggest that research demonstrating a statistically high incidence of SCI in patients who have been immobilised, simply suggests that spinal patients are appropriately treated with spinal immobilisation.
Anomymous can suggest that, but Anomymous is completely wrong.
If we give epinephrine to living heart attack patients and find that there is a high incidence of cardiac arrest after treatment with epinephrine, does that mean that we are doing something good by giving epinephrine to heart attack patients?
No.
We are making things worse by giving a dangerous treatment.
The patients who are not immobilized have much better outcomes.
–

Image credit from Voodoo Medicine Man.
–
To suggest a causal link is like saying hospitals are dangerous places because lots of people die in them.
Actually, that is the argument Anomymous is making, Anomymous just turned it around.
The patient died after the treatment – he must have really needed the treatment. If only we could have given him the treatment sooner (or given him more), he would still be alive.
Anomymous is making the mistake of assuming that the treatment is beneficial.
Anomymous is not providing any evidence that the treatment is beneficial.
–
The level of neurologic deficit was the only independent predictor of bad outcome (Table 4). We repeated this analysis using only the subset of patients with isolated cervical level deficits. We again failed to show a protective effect of spinal immobilization (OR 1.52; 95% CI 0.64-3.62; p = 0.34).[1]
What does that mean?
It means that even adjusting for differences in injuries, there was no benefit from spinal immobilization. Patients were much more likely to be disabled with spinal immobilization than without spinal immobilization.
This would be the same as adjusting for the differences in medical conditions when comparing patients in the hospital and outside of the hospital – the example given by Anomymous. If the patients in the hospital were still more likely to die after adjusting for illnesses, then the conclusion that hospitals are dangerous would be valid.
–
Similarly, I think ethical approval of a study evaluating the effects of not immobilising spinal patients might be hard to obtain – ‘Hmmm, 139 paralysed patients out of 150… I guess we were right all along…’
Why does Anonymous assume that this dangerous treatment (spinal immobilization) is beneficial in any way?
This is just wishful thinking.
Why should anyone believe Anonymous, who claims – without evidence – that a treatment that dramatically increases the rate of disability (according to the best available evidence) will actually prevent disability?
–
Of 334 immobilized patients with acute blunt traumatic spinal or spinal cord injuries, 21% had significant disability.
Of 120 not immobilized patients with acute blunt traumatic spinal or spinal cord injuries, only 11% had significant disability.
Is the better treatment hard to recognize?
That study that Anonymous claims would not be ethical? That study was already done.
Spinal immobilization failed.
–
Footnotes:
–
[1] Out-of-hospital spinal immobilization: its effect on neurologic injury.
Hauswald M, Ong G, Tandberg D, Omar Z.
Acad Emerg Med. 1998 Mar;5(3):214-9.
PMID: 9523928 [PubMed – indexed for MEDLINE]
.


check…and mate.
h dawg,
Thank you.
.
You keep using the same study in reference to “blunt” trauma…last I checked blunt trauma isn’t a catch all for all trauma.
Oh, so I get it now. We need to spinally immobilize the leg fracture from the press in the machine shop or the hockey player who fractures his arm from a puck striking it. Right?
CS,
This is what comes from the top doctors at PHTLS –
Prehospital spine immobilization for penetrating trauma–review and recommendations from the Prehospital Trauma Life Support Executive Committee.
Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE.
J Trauma. 2011 Sep;71(3):763-9; discussion 769-70. Review. No abstract available.
PMID: 21909006 [PubMed – in process]
Free Full Text PDF Download from http://www.ucdmc.ucdavis.edu/
–
While Dr. McSwain disagrees with me about immobilizing patients for blunt trauma, he was very upset when he learned that people are still being immobilized for penetrating trauma. The 7th edition of PHTLS stresses that spinal immobilization only considered appropriate when neurological deficits are present in the initial exam. Too many people are being killed by immobilizing penetrating trauma patients.
Eventually, they may admit that there is no evidence of benefit to blunt trauma patients, but there is a lot of tradition in immobilizing blunt trauma patients and we cannot expect them to move too quickly on this. After all, the motto is – First, Do no harm, unless it is a very traditional treatment considered to be the Standard Of Abuse.
Maybe in 5 years. Maybe in 10 years. Maybe in 20 years. Eventually, the evidence of harm and lack of evidence of benefit will convince doctors of the need to change – or maybe tort lawyers will start suing when EMS immobilizes patients who end up disabled. The lawyer for the EMS agency/EMS medical director would have to explain why this dangerous treatment is being used – without research to support long spine board immobilization and with research demonstrating harm. It should be an easy multi-million dollar case for the lawyer.
Who will respond to the research first, the doctors (PHTLS seems to set the standards, even if they deny setting standards) or the lawyers?
.
There is more evidence against routine immobilization than for it. In fact there is no evidence for it. Like too many things, it’s based on the EMS. Boogie Man, not medical science.
We’ve known since the Viet Nam war that even rifle caliber wounds to the head very, very rarely produce occult cervical injuries, and those that do are usually fatal in their own right.
My system gave up on immobilization of penetrating trauma patients unless there is evidence of neurologic injury years ago. When we put patients on boards it’s for ease of movement, not immobilization. We’ve yet to hear that we’ve had a negative outcome.
Yes, bullets can take strange paths, but if they cause spinal injuries, we know it immediately.
Even when there is injury, I don’t know of evidence that immobilization prevents further injury, let alone reduces the existing injury.
One of the reasons that doctors so love this procedure is that they are secure in the knowledge that they will neither have to inflict nor endure it.
Maybe we should require all doctors who want to be medical directors or medical control doctors to be immobilized per PHTLS standards, placed in an ambulance, driven around for 15 minutes and then left in a room in an ER for 2 hours.
That would change some attitudes.
I once heard a doctor that also happened to be a medical director respond to the question of whether or not EMS could use the same clearance protocols that the ER routinely uses to clear the spine and thus not inflict spinal immobilization on patients. The answer was no. Because, the patient might vomit and you don’t have the number of hands to roll the patient to the side and with them on a board one person can roll them to the side and maintain complete and total spinal immobilization. Go ahead, try and find a hole I haven’t poked in that argument. Dare you.
Can’t say, clowns will eat me,
Clearly, the treatment for nausea is intubation and suction as emesis prophylaxis.
But no sedation, because the intubated patient might stop breathing.
And think of the trauma! We can’t give a vasodilator to a trauma patient. What if the patient is bleeding? It is OK to mess around on scene crucifying the patient, but sedating the patient appropriately is unacceptable./
.
The problem with spinal immobilization is that it is based entirely on theory with no actual evidence that it works. The theory behind it is reasonable … keep the patient’s spine from moving, so that if an unstable spinal fracture is present there will be no further damage to the spinal cord.
However, the spinal immobilization that is used in the prehospital environment is not based on any actual evidence that it prevents disability due to spinal cord injury … nor does it actually fully immobilize the spine. I don’t care how skilled you are … applying a c-collar and putting someone on a backboard always requires at least some degree of movement of the patient’s spine.
It seems that the only reason we continue to do it is “because that’s the way it’s always been done.”
Prehospital RN,
Yes.
–
Exactly.
–
Unfortunately, that is one of the reasons, but people are starting to think about this.
Another reason is the fear of lawyers – and people will do all sorts of Ward Off the Lawyers dances to try to prevent themselves from being sued. Luck has more to do with being sued than anything else, but try explaining that to a superstitious Ward Off the Lawyers dance fan. They are not thinking. That is what happens when overwhelmed by fear. We shut down our rational processes and react reflexively – at the expense of the patient.
We engage in malpractice in order to protect ourselves from possible malpractice claims.
We are self-destructive superstitious primitives, willing to sacrifice our patients on the oxymoronic altar of defensive medicine.
.
Too Old To Work,
Exactly. It is based on the fear that if the patient really does have a spinal injury and we didn’t do something aggressive, then we weren’t trying. Better to do something dangerous (and stupid), than to be seen as not trying.
I prefer putting on a fancy headdress – not the Carmen Miranda thing, but something masculine – and chanting up a storm (oops, I keep confusing the rain dance with the no paralysis dance) – and chanting the spinal cord back to health, than this modern method of crucifixion.
–
The hubris of the Grand Inquisitor – safe from his own punishments.
–
Not every medical director –
Only those who think that spinal immobilization is defense against lawyers.
Only those who think that spinal immobilization is a good idea.
Only those who think that spinal immobilization is medicine.
Much as the doctor, who thinks that 2 mg of morphine is aggressive treatment of pain, changes his mind when he experiences severe pain. There is nothing wrong with telling doctors that they need to experience the pain they put patients through for no benefit before they subject any patient to the same abuse. If that does not teach them, maybe they are not smart enough to work in an ED.
.
If only the reactive, non-progressive medical directors were to experience a taste of their own medicine….hehehe.
Perhaps they have lost sight about why we do what we do: to care for the patients with the skills and tools we have to the best of our capability.
Ugh. With my elderly patients that would fall, I would routinely use a scoop to get them on the bed and then remove it, pad the sides of the stretcher with blankets to limit movement. I would always have a few newbies question my method. My rationale: By placing these patients on a LSB with full immobility precautions, you do more harm than good: Pressure ulcers, increased pain and stiffness, and with the older population you also run the risk of Rhabdomyolosis and a host of other complications. Our ER docs were great in supporting the decision. 9/10 the boards are removed immediately on handover anyway.
Mulitrauma from an MCA, different story. You adapt your treatment to the patient, not the patient to the treatment.
But what about when your medical director insists that you can’t do that regardless of whether or not the other doctors(even if it’s all of them) in the ER agree with your treatment because you have blasphemed the Holy Book of Protocol?
Can’t say, clowns will eat me,
They nail you to the backboard as punishment?
That is cruel and unusual punishment, but responses to blasphemy demonstrate who really is ethical and who will use any unethical tactic to defend the protocol, because the protocol is more important than the patient./
.
.
I take the lecture, walk out and know that I did the right thing for my patient. In my system, I live in Denver, CO, our doctors are usually okay with our treatment and encourage us to think outside of the box. If you have good rationale for what you did, then they usually will listen to you.
I have been on a backboard, I have neck injuries. I also have been improperly KED’ed. I know what it feels like and what it does to you. Not a good feeling.
Amy,
I like it.
I have been able to contact medical command to get permission to not break the patient’s bones on the backboard.
I have also called command and been greeted with, Please tell me that you have not placed this patient on a backboard.
We are supposed to at the minimum pad the backboard for the patient, so why doesn’t anyone get written up for transporting the little old lady with kyphosis and scoliosis and osteoporosis strapped to a board in a way that is designed to break her bones in order for her to fit the board?
Because we are afraid to think.
Thank you for thinking.
Thank you for caring for your patients.
.
Thank you. I try hard. I take patient advocacy very seriously. If it will hurt them more with no benefit to their future, shouldn’t there be an alternative?
Thanks for your blog, you make me think.
While our system does require the use of LSBs (and I agree with them for MVAs and other multisystem traumas), it’s perfectly acceptable to come up with a better idea for patients that would suffer from an LSB.
I had a contorted old lady who fell out of bed and was clearly injured. Trying to uncurl her onto an LSB would’ve been extremely painful and damaging. Instead, we wrapped the Ked around her and used caution while lifting and transporting. It worked wonders.
We do the same for unstable pelvises.
One of the other dangers is the patient, especially elderly patient, with a Hx of CHF or other respiratory ailment that can’t tolerate lying flat. You run the risk of taking a patient with a potential problem and converting them to a patient with an actual life threatening problem.
I forgot to mention earlier that the State of Maine has had a C-Spine evaluation protocol for ALL levels since 1995. During my infrequent trips to the state I have not noticed an epidemic of people in wheel chairs from their occult C-Spine injuries that were exacerbated by not being placed in a medieval torture device.
I recently got trained as a Wilderness First Responder (FR + Wilderness Protocols) and one of the things we covered was clearing the spine. The actual teaching of this took somewhere between 5 and 10 minutes (after all, you’ve pretty much done the same thing in a thorough head-to-toe), and then it went into our toolbox for every patient we practiced on after that.
Now that I’m reading around (thinking about going for EMT-B), it seems that everyone is required to backboard patients with spinal MOI regardless of whether they have signs+symptoms of spinal injury. So either there’s a fast, easy, relatively accurate way to assess for spinal injuries that can be taught to lay responders (because WFRs are considered lay responders in a wilderness context) but isn’t being used, or our instructors just taught us how to permanently diable everyone we meet out there.
I’m super new to this field, but that dissonance really bothers me.
I’m an EMT-B, Wilderness EMT, and MPIC certified. (This is not including my military SoP)
When you were trained as a WFR, you should have heard the statement that clearing the spine was considered a “wilderness only” skill (At least two hours away from definitive care is what I was told.) Outside of a specific set of circumstances, it’s to be considered outside your scope of practice.
Everyone in Maine from EMT-B up has been clearing C-spine in the field for at least ten years now.
That is statewide, and not limited to wilderness areas or wilderness EMT’s.
I clear C-spine every single day in Louisiana.
It may be out of the scope of practice for a First Responder of any stripe, but it is by no means beyond the scope of any EMT level.
Using common sense and a well-defined set of clearance criteria should not be beyond the scope of ANY pre-hospital provider. The only reason that it persists is dogma, superstition and unreasoning fear of legal liability.
Maybe I’m too jaded, but anyone that has been doing this line of work for longer than a couple of years has realized that spinal immobilization is nothing more than torture. Those that have been doing this line of work for more than a couple of years and still adamantly defend its use, are the very same knuckle dragging neanderthals keeping EMS in the dark ages.
My casual observations have brought me to the conclusion that the EMS personnel in the above mentioned adamant category fall into some distinct groups. The first (and possibly worst) perform (or threaten to perform) this ritual in order to punish patients over trivial (in their estimation) calls such as parking lot fender benders and same level slip/trip & falls. The next group that routinely bind up their patients are the ones that have been convinced that if it’s not written, you had better not do it. They’ve been so thoroughly indoctrinated/intimidated by the protocol Nazis, that they would probably have a seizure if you insisted on doing what was in the best interest of the patient. Then there is the group that know it serves no purpose and only perform the ritual haphazardly solely because it makes it easier to move and transfer the patient and reduces their chance of being called out by one of the above mentioned protocol Nazis. The last group are the ones that are quite simply “dumber than a bag of hammers”. There’s just no other way to put it.
Whew, I feel better now.
Yes, I agree. That being said, what about when you’re in an area where you wouldn’t be able to find work elsewhere in EMS if you do what’s best for the patient but doing so goes against your service/medical director/etc and they essentially threaten your job but tell you to provide great care which would involve not following the protocols they just told you to follow?
Do you do what’s right and lose your job and have to try to survive asking people if they’d like fries with that? Or do you go along, get along and probably get promoted to management? Or just say screw it all and go become a doctor yourself so that you can someday punish good medics?
I think the individuals that you’re describing are the ones paying attention to current research; challenging the staus quo as much as they can in their system; interacting with the ER docs that they transport their patients to and fostering relationships and trust with those doctors in order to perform their jobs better. I agree that there are times when we simply have to go along to get along. It sucks. I absolutely hate it when these situations come up. When these cases do crop up, I try to discuss them with some of the docs to get different takes on the situation. I use their input to try and avoid a repeat of the situation.
One thing that I’ve learned over time is that the better your documentation, the easier it is do what’s best for your patient and not what’s best for the protocol Nazis.
And yes, I am now in the process of moving up the evolutionary food chain 🙂
I agree. It’s hard to sit there and provide “treatment” because the protocol brown shirts, or the medical director or their flying monkey lackeys demand or the alternative of “Off with their heads!”(insert mental image of Helena Bonham Carter as the Red Queen here) shouted from the ivory tower of medical control for having violated the holy scripture of protocol. Only to at another time have the Red King come and tell you that what you want to do is right and he understands where you’re coming from and he agrees the holy scripture of protocol is in fact the true heresy but being the King he claims to be powerless to change it.
I get it, I’m adult enough, for a clown, to understand sometimes you have to bite your lip and just deal with it. That is until I find a way to make a better living doing less work, less liability and less danger. Until then, it’s one clowny day after another.
The study you cite, while very good at demonstrating that routine spinal immobilization is not necessarily good, IMHO does NOT prove your assertion that spinal immobilization is harmful. The data in that regard is very questionable. For example, the dependent variable was neurologic injury, not CHANGE in neurologic injury. For all we know, the U.S. patients were all much more heavily injured; in fact, it is reasonable to infer that based on the fact that a larger number of patients in Malaysia (16,600 vs 12,700) resulted in barely over a THIRD of total cases studied (120 vs 334). It is also impossible to tell if the injury/deficit was present on-scene or developed during transport.
As the study states, it is very problematic to have a true comparative study with the laws and public opinion as they are now. To be valid for EMS, a study needs to indicate the neuro status on-scene compared with after transport; otherwise it’s just guessing when and where the neuro damage was done.
mpatk,
This is the only study we have that compares spinal immobilization.
I have never stated that the study was perfect, but it is all we have and it does show that the patients immobilized did much worse.
I have been asking for more research on spinal immobilization.
The people opposing research that might show a benefit or safety are the advocates for spinal immobilization.
–
The number of participants is not a factor, since the percentage of patients harmed is doubled with spinal immobilization.
The risk of harm is doubled.
The other points are good reasons to demand further research.
–
In the absence of evidence of benefit, ANY evidence of harm is the best evidence we have.
Treatments that are not based on evidence should be dismissed without evidence.
The burden of proof is on those advocating for a treatment to demonstrate that the treatment is
1. Safe – there is no evidence of safety.
2. Efficacious – there is no evidence of efficacy.
3. Not harmful – there IS evidence of harm.
A study could be designed to contradict this study, but it is opposed by the advocates of spinal immobilization.
See also Answer to What is this Dangerous Treatment and How Long Did it Take to Stop Using it.
.