–
Dr. Ken Grauer wrote a couple of extended comments in response to Killing Patients Just to Get a Temporary Pulse With Epinephrine.
Dr. Grauer has provided some commentary on this on his web site – KG-EKG Press.
ISSUE #10: Should We Still Use Epinephrine for Cardiac Arrest?
So, how bad was epinephrine in this study?
–
Dr. Grauer writes –
I am not a statistician – and I admit to not understanding much of the technical jargon in the methodological portions of this manuscript – BUT – the cited “propensity score” data for Epi administration to my reading seems highly contrived – and I have trouble accepting this concept as being valid in this nonrandomized observational study …
I am not a statistician, either. However, the epinephrine group had a bunch of large advantages in this study.
–

Click on images to make them larger.
–
In spite of those large advantages, the only advantage to the no epinephrine group was in response times being 7:18 vs. 7:54, the unadjusted results showed that patients did better without epinephrine.
–
–
What did the 2010 ACLS Guidelines recommend about epinephrine before this study was completed?
It is reasonable to consider administering a 1 mg dose of IV/IO epinephrine every 3 to 5 minutes during adult cardiac arrest (Class IIb, LOE A).[2]
It is only reasonable to consider giving epinephrine.
Not – It is mandatory to consider epinephrine.
Not – It is reasonable to give epinephrine.
Definitely Not – It is mandatory to give epinephrine.
Certainly Not – It is unethical to withhold epinephrine.
Absolutely Not – Giving epinephrine will improve outcomes.
ACLS does not state any of that.
Deemphasis on Devices and Advanced Cardiovascular Life Support Drugs During Cardiac Arrest
At the time of the 2010 International Consensus Conference there were still insufficient data to demonstrate that any drugs or mechanical CPR devices improve long-term outcome after cardiac arrest.45 Clearly further studies, adequately powered to detect clinically important outcome differences with these interventions, are needed.[3]
Clearly further studies, . . . , are needed.
It looks as if the AHA (American Heart Association) is ready to give up on epinephrine in cardiac arrest unless someone provides evidence of actual benefit to real patients.
50 years of traditional use of epinephrine, unimpeded by a lack of evidence.
–
Thus, properly evaluating this traditional therapy now seems necessary and timely and should consist of a rigorously conducted and adequately powered clinical trial comparing epinephrine with placebo during cardiac arrest. Such a trial has previously seemed unethical, and investigators who have attempted to perform this comparison have received unwarranted criticism in their communities.17,19 While awaiting results of such a definitive trial, physicians and other practitioners involved in cardiac resuscitation must consider carefully whether continued use of epinephrine is justified.[4]
You will notice that the list of authors for the 2010 ACLS Guidelines includes the same Dr. Callaway who wrote this editorial. This should be a hint of what we can expect from the next change in the guidelines. Dr. Callaway is not the only doctor involved in writing the guidelines, but the ACLS Committee as a whole has been moving away from medications and has been emphasizing high-quality chest compressions.
Unless there is a miracle and a new study shows some benefit from epinephrine in cardiac arrest, I expect epinephrine to be removed from the next revision of the ACLS Guideline.
–
The 2015 ACLS Guidelines –
Epinephrine is only recommended for asthma and anaphylaxis.
Why?
Those are the only medical emergencies that have evidence of benefit from epinephrine.
No more voodoo.
–
Footnotes:
–
[1] Prehospital epinephrine use and survival among patients with out-of-hospital cardiac arrest.
Hagihara A, Hasegawa M, Abe T, Nagata T, Wakata Y, Miyazaki S.
JAMA. 2012 Mar 21;307(11):1161-8. doi: 10.1001/jama.2012.294.
PMID: 22436956 [PubMed – indexed for MEDLINE]
–
[2] Epinephrine
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science
Robert W. Neumar, Chair; Charles W. Otto; Mark S. Link; Steven L. Kronick; Michael Shuster; Clifton W. Callaway; Peter J. Kudenchuk; Joseph P. Ornato; Bryan McNally; Scott M. Silvers; Rod S. Passman; Roger D. White; Erik P. Hess; Wanchun Tang; Daniel Davis; Elizabeth Sinz; Laurie J. Morrison
Part 8: Adult Advanced Cardiovascular Life Support
Part 8.2: Management of Cardiac Arrest
Vasopressors
Free Full Text from Circulation with link to PDF Download
–
[3] Deemphasis on Devices and Advanced Cardiovascular Life Support Drugs During Cardiac Arrest
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science
Part 1: Executive Summary
John M. Field, Co-Chair*; Mary Fran Hazinski, Co-Chair*; Michael R. Sayre; Leon Chameides; Stephen M. Schexnayder; Robin Hemphill; Ricardo A. Samson; John Kattwinkel; Robert A. Berg; Farhan Bhanji; Diana M. Cave; Edward C. Jauch; Peter J. Kudenchuk; Robert W. Neumar; Mary Ann Peberdy; Jeffrey M. Perlman; Elizabeth Sinz; Andrew H. Travers; Marc D. Berg; John E. Billi; Brian Eigel; Robert W. Hickey; Monica E. Kleinman; Mark S. Link; Laurie J. Morrison; Robert E. O’Connor; Michael Shuster; Clifton W. Callaway; Brett Cucchiara; Jeffrey D. Ferguson; Thomas D. Rea; Terry L. Vanden Hoek
New Developments in Resuscitation Science Since 2005
Free Full Text from Circulation with link to PDF Download
–
[4] Questioning the use of epinephrine to treat cardiac arrest.
Callaway CW.
JAMA. 2012 Mar 21;307(11):1198-200. doi: 10.1001/jama.2012.313. No abstract available.
PMID: 22436961 [PubMed – indexed for MEDLINE]
Link to a free 6 1/2 minute recording of an interview with Dr. Callaway about this paper.
On the right side of the page, to the right of the First Page Preview, is a section with the title Multimedia Related by Topic. Below that is Author Interview. Below that is some information about the edition, . . . , and below that is an embedded recording of the interview. Press on the arrow to play. That has the recording of the interview with Dr. Callaway.
This is definitely worth listening to.
–
Hagihara, A., Hasegawa, M., Abe, T., Nagata, T., Wakata, Y., & Miyazaki, S. (2012). Prehospital Epinephrine Use and Survival Among Patients With Out-of-Hospital Cardiac Arrest JAMA: The Journal of the American Medical Association, 307 (11), 1161-1168 DOI: 10.1001/jama.2012.294
–
Callaway, C. (2012). Questioning the Use of Epinephrine to Treat Cardiac Arrest JAMA: The Journal of the American Medical Association, 307 (11), 1198-1200 DOI: 10.1001/jama.2012.313
.
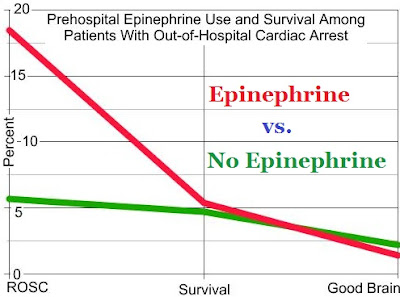


One thing I hope everyone can agree upon from the rather dramatic chart above: ROSC is NOT valid as a surrogate endpoint; and relying solely on ROSC will give a distorted, if not completely false, impression of any drug’s impact on actual survival.
The biggest message to take away from this paper IMHO is that there is no evidence of the effectiveness of epinephrine and studies need to be done on how effective epinephrine is in cardiac arrest. A true double-blind study, not a retrospective analysis. Retrospective analyses are good for indicating that more studies are needed, or for disproving some hypotheses (e.g. more ROSC = more survival is disproved here); but not sufficient to make definitive statements like epi is harmful. Only a clinical study with appropriate controls can make a claim such as that.