There si a discussion of the inevitable elimination of furosemide from the emergency drug list for CHF/ADHF (Congestive Heart Failure/Acute Decompensated Heart Failure). The only real surprise is that it has taken this long. The problems with furosemide have been documented since the 1970s.
This isn’t just a problem with CFH/ADHF. With the treatment of spontaneous pneumothorax, the problem has persisted, in spite of evidence, for even longer.
What is crucially needed here is what should have been done 40 years ago, which is a randomized controlled study of conservative observational management of primary spontaneous pneumothorax against what is currently the best evidenced intervention which is pleural aspiration.[1]
–
Nitro, morphine and furosemide: they’ve been the Holy Trinity of emergent treatment of acute CHF since the 1960s, but does this cocktail actually work?[2]
Déjà vu all over again?
–
Whatever the cause, CHFers rarely call EMS because their feet are swollen. They call because they can’t breathe, which is why we have traditionally considered CHF a cardiac disease disguised as a respiratory condition. The bulk of prehospital treatment of CHF is aimed at treating the primary clinical manifestation of left heart failure: cardiogenic acute pulmonary edema (APE).[2]
When their CHF/ADHF improves, their ankles will begin to improve, too. But we should not worry about their ankles when they can’t breathe. They don’t breathe through their feet.
–
Clinical presentation of acute pulmonary edema almost always manifests itself as severe respiratory distress, often accompanied by a constellation of associated signs and symptoms, including:
Profound hypertension (hallmark sign)[2]
This is why it is safe to use huge doses of NTG (NiTroGlycerin – GTN GlycerylTriNitrate in Commonwealth countries) for these patients, when they are hypertensive.
–
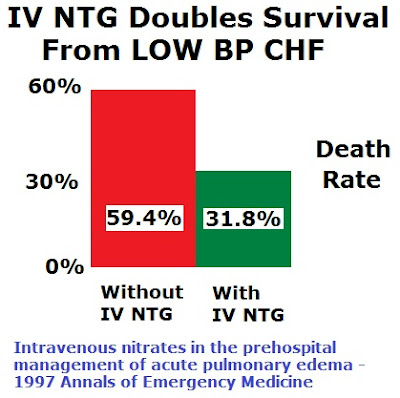
However, it also became apparent that higher doses of nitroglycerin resulted in significant dilation of the arterial system as well, reducing peripheral vascular resistance, increasing forward flow and, ultimately, decreasing workload for the weak and damaged left ventricle. This global vasodilatory effect of nitroglycerin has been shown to significantly reduce mortality in APE patients treated in the prehospital setting, and even hypotensive patients (systolic BP < 100) were shown to benefit from intravenous nitroglycerin.2 [2]
A systolic pressure less than 100? But we’ll kill the patients!
Actually, NTG is safe in much more hypotensive patients.
How hypotensive?
Is a blood pressure of 0/0 low enough?[3] 😯
Huge doses are safe.
–
We are supposed to be terrified of giving IV bolus NTG to hypotensive CHF/ADHF patients, but the death rate for hypotensive patients was cut in half by IV bolus NTG in this study.[4] NTG is not a new drug, we have just been too afraid to use enough.
–
Acute pulmonary edema, therefore, may likely be less of a fluid volume problem than a fluid distribution problem. There may be no excess accumulation of fluid needing to be diuresed; it is simply in the wrong place and needs to be distributed properly.[2]
Furosemide removes fluid, but only after the circulation returns to the kidneys. During critical illness, the body shunts circulation away from the kidneys. As with high-flow oxygen for chest pain, if the blood isn’t getting to the heart muscle, it does not matter how much oxygen is in the blood that isn’t getting where we want it. Like being in a traffic jam honking the horn, it may feel as if we are doing something, but we are only making things worse.
–
I prefer to keep treatment simple. Giving a bunch of drugs in a short period of time is a good way to make things a lot worse. This is kind of like the person who makes large adjustments to four different settings on a ventilator, but without reassessing at any point until after adjusting everything. Several drugs with varying durations of effect can also be a bad idea.
A lot of NTG. If you are uncomfortable, start off slowly, but if the blood pressure does not start to drop, keep increasing the dose. If this is CHF, small doses of NTG will probably have no effect on blood pressure. Expect the blood pressure to rise.
CPAP (Continuous Positive Airway Pressure), which makes it difficult to give sublingual NTG, but does not stop us from giving IV NTG – either as an infusion, which requires a pump, or boluses of the same doses we give under the tongue.
1 mg to 2 mg at a time – repeated every 3 to 5 minutes until symptoms improve.
This IS safe.
Go read the full article. Kelly and Gene know what they are writing about.
–
Footnotes:
–
[1] Spontaneous pneumothorax: time for some fresh air.
Simpson G.
Intern Med J. 2010 Mar;40(3):231-4. Review.
PMID: 20446970 [PubMed – indexed for MEDLINE]
An excellent, but mostly unappreciated, review of the problems with the Standard Of Care for spontaneous pneumothorax. Not that much different from the mythological treatment that persists in so many other areas of medicine.
–
[2] CHF Treatment: Is Furosemide on the Way Out?
Created: June 1, 2012
by Steven “Kelly” Grayson, NREMT-P, CCEMT-P and William E. (Gene) Gandy, JD, LP,
EMS World
Article
–
[3] High dose nitroglycerin treatment in a patient with cardiac arrest: a case report.
Guglin M, Postler G.
J Med Case Rep. 2009 Aug 10;3:8782.
PMID: 19830240 [PubMed]
Free Full Text from PubMed Central
–
[4] Intravenous nitrates in the prehospital management of acute pulmonary edema.
Bertini G, Giglioli C, Biggeri A, Margheri M, Simonetti I, Sica ML, Russo L, Gensini G.
Ann Emerg Med. 1997 Oct;30(4):493-9.
PMID: 9326864 [PubMed – indexed for MEDLINE]
.


It’s so sad that people continue using lasix despite the evidence. Luckily we are going away from it as a service because if not it would continue. I love seeing people give huge doses and a non rebreather. My last partner was surprised how well nitro and a cpap worked and after some explaining he has now convinced his full time partner to go the nitro cpap route and not to play around with lasix.
CPAP (Continuous Positive Airway Pressure), which makes it difficult to give sublingual NTG, but does not stop us from giving IV NTG – either as an infusion, which requires a pump, or bolues of the same doses we give under the tongue.
Difficult, yes, but not impossible to give SL NTG with CPAP. Just incredibly impractical, but the key is to get the first SL dose in before applying CPAP. Sounds incredibly simple, I know, but the incidence of medics putting the mask on first without NTG first is actually rather high…
In NH, the service I work for carries Tridyl (the trade name for IV NTG – don’t know if this is the correct spelling), and it is not uncommon to have to start a drip when dealing with someone who is in acute CHF. NTG and CPAP are the first two interventions we use, and they are quite effective. Morphine is still in the protocol, but it is listed after the first two have been done. Lasix is last on the list and it is a medical control option only – we no longer have standing orders for it.
In MA, on the other hand, we do not carry Tridyl, but we do carry nitro paste. In my own experience, I’ve found this to be nearly as effective as IV Tridyl. Part of the problem we have in MA, at least in the service I work at, is the only trucks that have IV pumps are Crtical Care Transport vehicles. No other trucks have them. Consequently, our medical director specified paste instead of Tridyl.
The other parts of the protocol I mention are nearly identical in MA and NH.
My inclination is to think that whether or not Tridyl is available is an issue of it being a local option where the medical director has the final say.
Furosemide removes fluid, but only after the circulation returns to the kidneys. During critical illness, the body shunts circulation away from the kidneys. As with high-flow oxygen for chest pain, if the blood isn’t getting to the heart muscle, it does not matter how much oxygen is in the blood that isn’t getting where we want it. Like being in a traffic jam honking the horn, it may feel as if we are doing something, but we are only making things worse.
The other consideration with any type of diuretic is the potential for introducing electrolyte imbalances. While I have never personally seen this occur, nor do I have any quantifiable evidence of this happening, considering what the mechanism of action is of any non potassium-sparing diuretic is (loop diuretics and thiazides come to mind almost immediately), in my mind this is a logical response of the effects diuretics have. And, at least anecdotally, there have to be instances of this that have occurred. I wouldn’t be surprised to find documented cases as well.
1 mg to 2 mg at a time – repeated every 3 to 5 minutes until symptoms improve.
This IS safe.
Yes – it is.
Excellent post.
The anonymous post was mine, Tim – I forgot to sign it.
I will say again that yours (and Kelly’s) was a well-written explanation of the benefits of NTG in CHF. If you have no objection I would like to forward it along to someone I know who still harps on the use of Lasix as a first-line intervention for treating CHF – hopefully it will give them something to consider next time they encounter someone who is this sick.
I believe it was five years ago that Lasix was removed from our standing orders for CHF, along with Morphine. Lasix was removed from our drug bags a year after that and Morphine was removed two years ago. NTG and CPAP are proven treatments and I have seen those patients transform in short order right in front of my eyes. My standing orders call for SL NTG q 5min until CPAP can be spplied then a NTG drip 50mcg/min titrated to 200mcg/min as fast as possible as long as BP is greater than 100 systolic. I have had nurses freak out when I give a report of a nitro drip at 50mcg/min, that is only about half the nitro they get with repeating SL doses q 5min. Without the lasix you do not have to worry if the patient is volume depleated or septic.
Personally I love my NTG drips and use them frequently. CHF gets nitro, chest pain relieved with SL Nitro gets a drip. Just as I love my CPAP for difficulty breathing. We finally have treatments that work and do not mask problems and only make someone feel better, they make them better and that is why I became a Paramedic. Not to make me feel better because I could give some cocktail but, to make my patient better.
The problem is not a question of NTG and CPAP working as treatments for these patients but, education of Paramedics of why we need to change. But, that is one of the biggest problems in EMS, thinking change is bad and the mentality of taking away drugs equals you do not trust the Paramedic to make a clinical decision when in fact, it may have everything to do with a better treatment. As far as Lasix goes I cannot think of any condition that my patient would be harmed from not having it in the 30 min I have them. Even if there were conditions that required the use of a diuretic there are much faster acting and better drugs we should be using.
In my county, we carry nitro paste for “long transport times” and traditional SL NTG for normal use. The Critical Care units (with RN) carry IV NTG. There is a provision for “expanded scope” paramedics to administer IV NTG during transfers; but there is very little interest because it’s approved for IFTs only and medics who get that certification will end up being the designated IFT unit.
Does anyone out there give NTG as an IV bolus? Just curious what form that would take (concentration, bolus size in mL, single-use vs. multi-use vials, etc…).
Frusemide is way old school, its great for chronic heart failure not so much for acute heart failure
Chronic hypervolaemia vs acute fluid shift are two different things so you cannot extrapolate what is good for the one as being good for the other
Many services worldwide have withdrawn frusemide, New Zealand did so in September 2011 and I say good riddance