How do we determine which patients go to a trauma center?
Too often by MOI (Mechanism Of Injury).
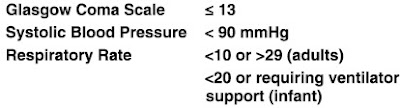
Physiologic criteria are not too bad and involve some assessment of the patient.
Notice that the GCS (Glasgow Coma Score) is not just for a history of a loss of consciousness or for not being fully oriented.
Anatomic criteria are also not too bad and similarly involve some assessment of the patient.
Mechanism Of Injury is where the most disagreement arises and I have had some entertaining conversations with trauma doctors, but far more disagreement with those doctors who have only anecdotal trauma experience.
The MOI that accurately predicts trauma center need remains a controversial debate within the trauma community. One specific example of this controversy is the rollover mechanism. Single-center experience suggests rollover is not predictive of severe injury, while a review of a large government database suggests otherwise.13,14 [1]
This study excluded everyone who met physiologic or anatomic criteria in order to assess the ability of MOI alone to identify need for a trauma center.
Trauma center need was defined as death, Injury Severity Score (ISS) of more than 15, blood transfusion in the emergency department (ED), intensive care unit (ICU) admission, pelvic fracture, need for laparotomy/thoracotomy/vascular surgery within 24 hours of arrival, two or more proximal long bone fractures, or neurosurgical intervention during admission.[1]
Some of those duplicate anatomic criteria, but they appear to refer to pelvic fractures and pairs of long bone fractures that were not identified by EMS and were not documented by EMS as criteria for trauma activation.
How much risk of death is there for these mechanism-only patients? We do not know, but only 0.3% died in the hospital.
How many of them would have been triaged as trauma alerts by a good assessment?
The biggest problem with this paper is that it is not able to tell us whether these patients would have been triaged as trauma alerts without MOI criteria to point to for documentation.
The goal of every trauma center is to treat as many seriously injured patients as possible, while directing care of the less severely injured to community hospitals. To achieve this goal, the ACSCOT suggests that an overtriage rate of 50% is acceptable to maintain an undertriage rate of 5% or less.15[1]
Our overtriage rate of 77% was higher than that which is considered acceptable by the ACSCOT. The overtriage rate in this study is consistent with that noted in other studies, which used the 1999 guidelines for evaluating MOI in prehospital triage, which ranged from 75% to 91%.21–24 [1]
In 2006, our system stopped requiring trauma center transport of patients meeting Step 3 criteria.[1]
Step 3 is MOI.
Requiring medical command permission to fly patients meeting MOI criteria in Maryland led to an apocalyptic prediction from the top trauma doctor.
“Whenever someone says they want to ratchet it back,” says Dr. Thomas M. Scalea, physician in chief at Shock Trauma, “I tell them ‘OK, how many people can die next year to make that worthwhile?’”[2]
There have not been any reports of increases in the fatality rate with that change.
How did the MOI criteria do?
Wrong question. Since they eliminated the use of MOI criteria in this system, we have a strong hint.
Orthopedic operations were the most common procedures performed on those patients transported from the ED to the operating room (289 patients, 68%). Eighteen patients (4%) did require a laparotomy, thoracotomy, or vascular procedure directly from the ED. Of those requiring laparotomy (11 patients, 3%), 2 were to repair a liver laceration, 2 for splenectomy, and 4 were intestinal repairs/resection. Three nontherapeutic laparotomies were performed.[1]
Those numbers are better than what I would expect. I used to work in a trauma center that had less than 5% of trauma alert patients go to surgery in any kind of rush. Surgery is not the only criterion for whether the trauma center is an appropriate destination.
Significant MOI predictors of trauma center need include death in the same passenger compartment, ejection from the vehicle, extrication time of more than 20 minutes, fall from more than 20 feet, and pedestrian thrown/runover.[1]
Those are the criteria they think have some predictive value.
Here are the ones that are old wives’ tales.
Criteria that did not meet our definition of trauma center need were vehicle intrusion, vehicle rollover, speed of more than 40 mph, autopedestrian/autobicycle of more than 5 mph, and both of the motorcycle crash criteria.[1]
Separation of the motorcyclist from the motorcycle is not a bad sign, but it shows that the MOI criteria were written by someone who does not understand motorcycles. In a crash, remaining inside a car/truck is protective, but remaining attached to the outside of a motorcycle is almost as bad as being strapped to the outside of a car/truck. This is the reason motorcycles do not have seat belts. Motorcycles do not offer physical protection. The protection is in the increased maneuverability and the ability of the rider to avoid getting in trouble. A motorcycle crash at highway speed is only bad if you are hit, hit something, or if you are not wearing protective gear.
How much better would a good assessment be at correctly identifying patients who have critical injuries?
How much worse would a good assessment be at correctly identifying patients who have critical injuries?
A good assessment would require good education and good oversight.
As with other interventions, this should be studied prospectively.
–
Footnotes:
–
[1] Not all mechanisms are created equal: A single-center experience with the national guidelines for field triage of injured patients.
Stuke LE, Duchesne JC, Greiffenstein P, Mooney JL, Marr AB, Meade PC, McSwain NE, Hunt JP.
J Trauma Acute Care Surg. 2013 Jul;75(1):140-5.
PMID: 23940858 [PubMed – indexed for MEDLINE]
–
[2] Advantages of medevac transport challenged
Baltimore Sun
October 5, 2008
Article
–
Stuke, Lance E. MD, MPH; Duchesne, Juan C. MD; Greiffenstein, Patrick MD; Mooney, Jennifer L. MD; Marr, Alan B. MD; Meade, Peter C. MD; McSwain, Norman E. MD; Hunt, John P. MD, MPH (2013). Not all mechanisms are created equal: A single-center experience with the national guidelines for field triage of injured patients. Journal of Trauma and Acute Care Surgery, 75 (1), 140-145 DOI: 10.1097/TA.0b013e3182988ae2
.




[…] Jefferson County the safest place in the North Country? « The In BoxNot all mechanisms are created equal | Rogue MedicH5N1: Syria: Torture as a public health issueSteve King takes on critics of his […]