Start a conversation on use of back boards in almost any EMS group and expect someone to say that, based entirely on mechanism of injury, the uninjured patient must be strapped to a back board Just to Be Safe.
Is it safe?
No.
Where is the evidence of safety?
Where is the evidence of benefit?
What we get is just the ignorance-based bias of the person who has no understanding of safety.
RESULTS:
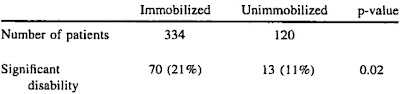
There was less neurologic disability in the unimmobilized Malaysian patients (OR 2.03; 95% CI 1.03-3.99; p = 0.04). This corresponds to a <2% chance that immobilization has any beneficial effect. Results were similar when the analysis was limited to patients with cervical injuries (OR 1.52; 95% CI 0.64-3.62; p = 0.34).[1]
a <2% chance that immobilization has any beneficial effect.
Less than 2% chance of any benefit?
Roulette wheels have better odds playing just one number. It is reckless to bet on a single number in roulette (the only safe bet is to be the house, but that is a different topic). This is being reckless and irresponsible with our patients.
Why do we see gambling on the extreme long shot as safe?
Maybe because we are not gambling with our own disability.
We are betting our patients’ disability on our ignorance.
Is that safe for the patient?
The same study showed that those with unstable spinal injuries were twice as likely to be disabled if they were strapped to back boards.

Image credit from Voodoo Medicine Man.
The study is not definitive, but we are just guessing about what might work, based on an ancient hunch. We have no clue.
It is time we found out what works.
It is time we admit that we do not know what works.
We are clearly demonstrating that we are clueless about what safe means.
The standard of care has changed.
Spinal precautions can be maintained by application of a rigid cervical collar and securing the patient firmly to the EMS stretcher, and may be most appropriate for:
- Patients who are found to be ambulatory at the scene
- Patients who must be transported for a protracted time, particularly prior to interfacility transfer
- Patients for whom a backboard is not otherwise indicated[2]
This is from the people who write the PHTLS (PreHospital Trauma Life Support) and ATLS (Advanced Trauma Life Support) guidelines as well as from the NAEMSP (National Association of EMS Physicians).
Do we want to go to court and face experts who will say this about back boards just to be safe –
We don’t do that any more.
We learn from our mistakes.
Is that safe?
Isn’t it time we stopped encouraging people to make mistakes that harm our patients?
–
Footnotes:
–
[1] Out-of-hospital spinal immobilization: its effect on neurologic injury.
Hauswald M, Ong G, Tandberg D, Omar Z.
Acad Emerg Med. 1998 Mar;5(3):214-9.
PMID: 9523928 [PubMed – indexed for MEDLINE]
Free Full Text from Academic Emergency Medicine.
–
[2] EMS spinal precautions and the use of the long backboard.
[No authors listed]
Prehosp Emerg Care. 2013 Jul-Sep;17(3):392-3. doi: 10.3109/10903127.2013.773115. Epub 2013 Mar 4.
PMID: 23458580 [PubMed – in process]
Free Full Text in PDF Download format from NAEMSP.
.

Subscribe to RogueMedic.com