
And the Grinch, with his Grinch-feet ice cold in the snow, stood puzzling and puzzling, how could it be so?
It came without
ribbonsepi.It came without
tagsamio.It came without
packagesoxygen,boxestubes or bags.And he puzzled and puzzled ’till his puzzler was sore. Then the Grinch thought of something he hadn’t before.
Maybe
Christmasliving, he thought…doesn’t come from astoredrug.Maybe
Christmasliving, perhaps…means a little bit more!
With apologies to Dr. Seuss (Theodore Geisel) for the modification of his parable.
There are important differences between the minimal criteria for life and the criteria for a meaningful life. Many of us don’t like to think about that, because many of us don’t like thinking. Thinking can be hard. Making excuses for not thinking – priceless (at least, as long as you don’t think about it).
We have been focusing on the least honest way of reporting outcomes – a pulse – Oooh!, or maybe even 30 days of a pulse – Oood-Ahhh! After all, reality does not support continuing to do what we have been doing. If we admit that we have been causing harm, then we may have to take responsibility for our actions.
We do not want to take responsibility for our actions. We were only following orders.
Doctors, PAs (Physician Assistants), NPs (Nurse Practitioners), nurses, paramedics, EMTs, techs, . . . do not want to take responsibility for what we get paid for. Accountability is for people who think – not for us.
We have blamed science/evidence for requiring that we confront reality. As explained by Dr. Seuss, we want simple answers that do not require understanding. Give us algorithms to mindlessly follow. Give us mnemonics.
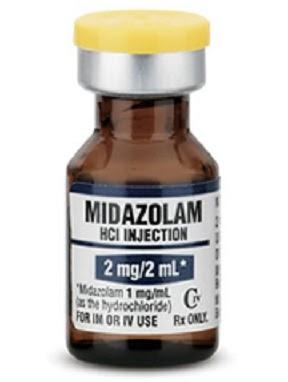
We have been giving epinephrine (adrenaline in Commonwealth countries) for over half a century with no evidence of safety or improvement in the outcome that matters most.
Why?
We haven’t wanted to know.
The first study to look at the effect of placebo vs. epinephrine on neurological survival was cut short – with only a tiny fraction of what would be needed to produce any kind of statistically useful information, except for some of the true believers, who made the same kinds of mistakes that have been made for other discarded treatments – treatments discarded due to failure to work, discarded due to harm, or discarded due to both.
Don’t study this. Just believe. Belief makes us feel good. Attack science for encouraging understanding.
This study was designed as a multicentre trial involving five ambulance services in Australia and New Zealand and was accordingly powered to detect clinically important treatment effects. Despite having obtained approvals for the study from Institutional Ethics Committees, Crown Law and Guardianship Boards, the concerns of being involved in a trial in which the unproven “standard of care” was being withheld prevented four of the five ambulance services from participating.[1]
In addition adverse press reports questioning the ethics of conducting this trial, which subsequently led to the involvement of politicians, further heightened these concerns. Despite the clearly demonstrated existence of clinical equipoise for adrenaline in cardiac arrest it remained impossible to change the decision not to participate.[1]
What was the conclusion produced by the Jacobs study?
CONCLUSION: Patients receiving adrenaline during cardiac arrest had no statistically significant improvement in the primary outcome of survival to hospital discharge although there was a significantly improved likelihood of achieving ROSC.[1]
As the homeopaths put their spin on studies that do not really support their claims, people who do not understand science put similar spin on the results of this. For example, if you take a Bayesian approach[2], but distort it to mean that you give extra weight to everything that supports your belief and take away credit from everything else, you can claim that this is an example of science proving that epinephrine works.
Another way of doing this is to claim that you don’t give the 1 mg dose of epinephrine, therefore the study does not apply to your patients. After all, you are just engaging in a poorly documented, unapproved study, which allows you to think of the survivors as examples of the drug working and make excuses for the rest. Of course, if you don’t give the 1 mg dose of epinephrine, is there any evidence that your treatment is safe or effective? No.
Rather than insisting that this method of dosing patients be studied, in order to determine if it really is safe or if it really is effective at anything other than getting a pulse in a brain-dead body, claim to be ahead of the science.
Why find out what is really best for the patients, when there are so many ways of declaring victory and running away?
In 2018, we had the results of the next study of placebo vs. adrenaline (epinephrine in non-Commonwealth countries, but only Commonwealth countries have bothered to do the research). The conclusion was the same as the conclusion for the only previous study.
CONCLUSIONS: In adults with out-of-hospital cardiac arrest, the use of epinephrine resulted in a significantly higher rate of 30-day survival than the use of placebo, but there was no significant between-group difference in the rate of a favorable neurologic outcome because more survivors had severe neurologic impairment in the epinephrine group.[3]
Has anyone else stated that the use of epinephrine should be limited to controlled trials?
Not that I know of.
Everyone else seems to be claiming that giving smaller boluses of epinephrine. or giving titrated infusions of epinephrine is different. Some claim that it is nihilism to refuse to believe in their slightly different treatment – at least until there is undeniable evidence of lack of benefit, or undeniable evidence of harm, or both.
Requiring evidence of benefit, before using a treatment on a patient is being reasonable.
Using inadequately studied treatments on people when they are at their most vulnerable is not good medicine.
A doctor’s oath to Apollo does not include a requirement to perpetuate dogma, but medicine is only slowly starting to focus on what is best for patients, rather than what is best for appearances.
Dr. Ryan Jacobsen addressed a similar dogma, when he got rid of the long spine board in the system where he was medical director. His description of the evidence applies to epinephrine (bolus, mini-bolus, infusion, patch, inhaler, down the tube, oral, whatever) –
Other than historical dogma and institutional EMS medical culture we can find no evidence-based reason to continue to use the Long Spine board epinephrine as it currently exists in practice today.[4]
I changed EMS to medical and the Long Spine board to epinephrine.
We have good evidence that if your loved one is a laboratory pig, rat, dog, . . . we can kill them and get them back neurologically intact with epinephrine – and with other treatments that have been discarded because they do not have the same effect on humans as on lab animals.
Let us treat your loved ones like the lab animals we think they are.
Don’t use EBM (Evidence-Based Medicine), because belief is more important than reality.
The world is a comedy to those that think; a tragedy to those that feel. – Horace Walpole.
Keep thinking. Keep demanding evidence. After the nonsense being preached by the believers is exposed, we can improve the outcomes for our patients, because medicine is about doing what is best for the patient, and not about protecting the dogma.
–
Footnotes:
–
[1] Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial
Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL.
Resuscitation. 2011 Sep;82(9):1138-43. doi: 10.1016/j.resuscitation.2011.06.029. Epub 2011 Jul 2.
PMID: 21745533
Free Full Text PDF Download from semanticscholar.org
–
[2] Bayesian inference
Wikipedia
Article
–
[3] A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest.
Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O’Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC2 Collaborators.
N Engl J Med. 2018 Aug 23;379(8):711-721. doi: 10.1056/NEJMoa1806842. Epub 2018 Jul 18.
PMID: 30021076
–
[4] Johnson County EMS System Spinal Restriction Protocol 2014
Ryan C. Jacobsen MD, EMT-P, Johnson County EMS System Medical Director
Jacob Ruthsrom MD, Deputy EMS Medical Director
Theodore Barnett MD, Chair, Johnson County Medical Society EMS Physicians Committee
Johnson County EMS System Spinal Restriction Protocol 2014 in PDF format.
.











Subscribe to RogueMedic.com