
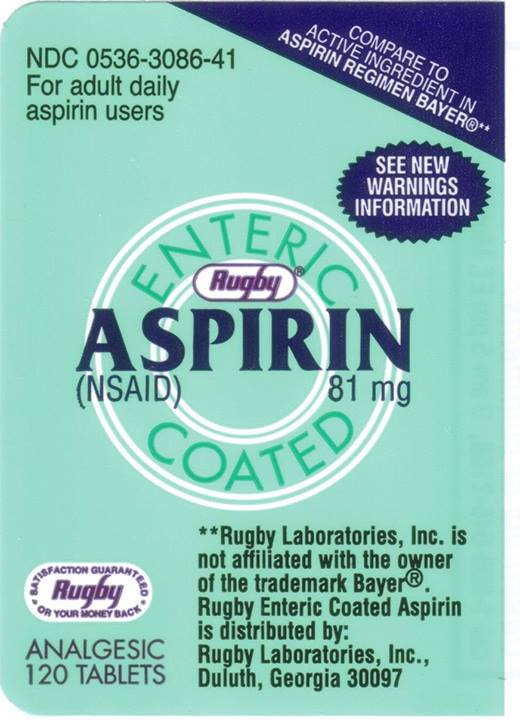
Last week the FDA (Food and Drug Administration) sent out a safety announcement about a recall of Rugby label Enteric Coated Aspirin Tablets, 81 mg, Lot 13A026.
The package does not contain 81 mg aspirin, but actually contains 500 mg acetaminophen (Tylenol), which is a much larger dose and is in many other over the counter medicines, such as cough and cold medicines. Almost all of these medicines contain a full adult dose of acetaminophen in addition to whatever the active ingredient is (guaifenesin, dextromethorphan, et cetera).
Consumers may be inadvertently taking Acetaminophen 500 mg instead of Enteric Coated Aspirin 81 mg which may cause severe liver damage to those who take other drugs containing acetaminophen, consumers who take 3 or more alcoholic drinks every day, or those who have liver disease. The labeled directions instructs patients to take 4-8 tablets every 4 hours, but not more than 48 tablets in 24 hours. Consumers who take 48 tablets daily of the defective product may be ingesting up to 24,000 mg of Acetaminophen, which is about six times the maximum recommended daily dose of acetaminophen (4,000 mg).[1]
Taking more acetaminophen than needed is not safe because of this duplication of doses. The liver may be able to remove the current amount of acetaminophen we are consuming (intentionally and unintentionally), but an extra half gram of acetaminophen may result in a toxic dose.
Some people only take 81 mg enteric coated aspirin on a daily basis for its antiplatelet effects, but the package recommends a lot more.
“It’s not an uncommon overdose,” said Dr. Corey Slovis, who heads the department of emergent medicine at Vanderbilt University Medical Center in Tennessee. “We hate Tylenol overdose because they’re the silent overdoses.”
Slovis said patients who overdose on acetaminophen often don’t feel sick right away, unless they’ve taken a massive dose that induces vomiting within six hours. Instead, many patients who overdose on acetaminophen don’t see a doctor for more than two days because they feel fine at first. When they finally get to Slovis, they’re often jaundiced and experiencing the early signs of liver failure.
As such, this kind of overdose could result in liver failure, the need for a transplant or death, Slovis said.[2]
The pills are probably larger than the normal aspirin pills, but if you are unfamiliar with the product, you would not recognize the difference. Taking a handful (4-8 tablets every 4 hours, but not more than 48 tablets in 24 hours) of pills at a time is probably not a good idea, regardless of the label instructions.
“Did he take six pills or only five?” Well, to tell you the truth, in all this excitement I kind of lost track myself.[2]
We have trouble counting beyond three.
–
Footnotes:
–
[1] Advance Pharmaceutical Inc. Issues Voluntary Recall of One Lot of Enteric Coated Aspirin Tablets, 81 mg, Due to Health Risk
Recall – Firm Press Release
FDA
Recall notice
–
[2] Aspirin Recalled Over Bottle Mix-Up
Sydney Lupkin (@slupkin)
ABC News
Article
–
[3] Dirty Harry (1971)
Quotes
IMDb.com
Quote
.










Subscribe to RogueMedic.com