There is also a comment from steve mauch on Two Children Abducted by EMS Helicopter for One Laceration that deserves comment.
Rouge, I see what you’re getting at, but the problem is not so much with the medic, its what/how he was taught. If in his area they are taught if you see skull you fly, then he did everything right.
Exactly.
That is what I am criticizing.
We are supposed to be doing what is best for the patient.
We are not supposed to be blindly following protocol, nor blindly following the local culture of fly everyone and let the trauma center discharge them right away.
We need to hold the medical directors and the EMS agencies accountable for this ridiculous approach to patient care.
Where is your outcry against the flight crew that made the decision to fly the second child?? Why not crucify the flight nurse too?!
It was not my intent to crucify the medic.
It is my intent to crucify the system.
I just need some people with hammers and nails and we can nail the system to a Star of Life. 😉
OK. I will settle for metaphorical crucifixion, but we didn’t have to settle for metaphor in the good old days.
I agree with rick in the fact that we should not be ridiculing each other, we get enough of that.
Sometimes ridicule is an excellent way to expose a problem.
Again, I was not focused on the medic, but on the actions that are commonplace in EMS.
Look at that mechanism!
We can’t be out of service for an hour! What if a call comes in and our dangerous neighboring service has to cover for us? Many of the people in the neighboring service work for both EMS services, because that is the way EMS works. So how dangerous is the neighboring service, if they have the same employees?
This encourages us to take a helicopter out of service for real emergencies, so that we can fly someone for vehicular damage, yet vehicles are designed to deform to protect the occupants of the vehicle – and that kind of design works very well.
My response to the doctors in the trauma center who have questioned me about why I did not fly a patient, why I did not call for a trauma alert, and/or why we took our time driving with traffic, rather than using lights and sirens is this –
Assess the patient and tell me what you find that is unstable, then we will talk.
I also am familiar with the research. There is no valid research that supports flying patients within a 45 minute drive of a trauma center.
There is no valid research supporting the idea that we are not using HEMS enough.
The helicopters are often in the wrong place. Many are close enough to the trauma centers that EMS should be driving patients, but that is not where a helicopter would make a difference in outcomes. Helicopters make a difference in outcomes for unstable patients who are well over an hour drive time from the trauma centers.
We are encouraging the helicopters to flock near the trauma centers, so that they can service the medical directors who write mechanism-only flight protocols that endanger patients.
Maryland changed their protocols so that medical command permission is required for a mechanism-only flight. Helicopter transports were cut by over half. Where are the dead bodies that Dr. Thomas Scalea predicted would be the result of this cut in flights?
But I agree with you that issues DO need to be addressed, but we need to look at the initial educators. As a fairly recent paramedic graduate, I can tell you that medics are being taught to be cookbook medics, we are not taught to think.
I agree.
But, each paramedic program is different.
We need to encourage those medic programs that do a great job. There are many out there.
We need to discourage those medic programs that teach people to be protocol technicians, IV technicians, monitor technicians, alarm technicians – Oh, look! The asystole alarm is going off. I need to start CPR. There are many out there.
[youtube]sao-uEKgJ6Q[/youtube]
How much have we changed from the days of calling for orders and being told to give one amp of the yellow box?
If we do not understand pharmacology, we do not understand the most important part of pharmacology – when not to give a drug.
The same is true for procedures. We need to understand when not to use a procedure. Defibrillation, as in the video, or cricothyrotomy, or intubation, or synchronized cardioversion, . . . .
When needle decompression is used, the use almost always appears to be inappropriate.
Needle decompression does save lives when used appropriately.
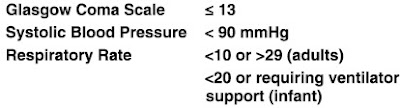
Click on the image to make it larger.[1]
The chart is for all patients stuck in the chest at least once with a needle in an attempt to decompress a suspected tension pneumothorax.
Many patients never had any kind of pneumothorax.
Was needle decompression used appropriately on any of these patients?
Maybe. Maybe not. We do not know.
It seems that many in EMS need a lot of work in learning when not to attempt needle decompression.
One of the biggest things I recall is SVT. I was “taught” greater than 150=SVT. I went on thinking this was fact. I was not taught svt is a class of rhythms, not a rhythm by itself.
SVT – SupraVentricular Tachycardia.
The sinus node is supraventricular.
Sinus rhythms do not benefit from adenosine or synchronized cardioversion.
Do not blame the medic for not knowing what someone else never took the time to pass along.
Yes and No.
We need to take responsibility for our own education.
Education does not stop once we put on a patch or get authorized to work on our own.
I was supposed to be writing about the presentations at EMS Expo this week, but it is looking as if that will be next week. If we attend EMS conferences, we can learn about the things our instructors misinformed us about.
Backboards probably do more harm than good, especially for the patients with unstable spinal injuries.
Helicopters do save lives, but probably only for unstable trauma patients over an hour from the trauma center.
How to interpret 12 lead (and 15 lead and 18 lead, . . .) ECGs and how to identify unusual rhythms.
Now I am off to once again demonstrate that a heart rate faster than my calculated maximum heart rate is possible and can still be sinus tachycardia. When I wake up, my heart rate will be a respiratory arrhythmia sinus bradycardia. All of these are arrhythmias/dysrhythmias, but they are not bad rhythms and they are not the absence of rhythm.[2]
These arrhythmias/dysrhythmias are better than normal sinus rhythm.
Arrhythmias/dysrhythmias are treatable, but most do not benefit from treatment.
Should anyone ever use the term normal sinus rhythm?
What do we base normal on?
Does that mean that the patient’s heart is healthy?
How much beat-to-beat irregularity is permitted while still calling the rhythm normal?
What is the difference between normal and healthy?
If a patient is having a normal episode of angina, is that a good thing?
If a patient is having a normal seizure, is that a good thing?
If a patient is having a normal case of hypoglycemia, is that a good thing?
Based on what?
We often use terms we do not think about. Does that mean that it is not normal for us to think?
Is normal good?
In all of that I forgot to mention, I agree that they should not have been flown, ESPECIALLY since mom was against it, but I wasn’t there and it wasn’t my call. I do think way too many people are flow, and even more people are backboarded that don’t require it. We need to improve critical thinking and assessments BEFORE applying devices and treatments, but that’s a whole new blog!
Again, this is about highlighting the problem, not the person.
We have a big problem. Making a scapegoat out of one individual does not change the problem.
–
Footnotes:
–
[1] Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study.
Blaivas M.
J Ultrasound Med. 2010 Sep;29(9):1285-9.
PMID: 20733183 [PubMed – in process]
Free Full Text from J Ultrasound Med.
When Should EMS Use Needle Decompression
Rogue Medic
Thu, 10 Nov 2011
Article
Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study – Full paper
Rogue Medic
Mon, 14 Feb 2011
Article
Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study – abstract
Rogue Medic
Tue, 07 Sep 2010
Article
–
[2] dys-
The Free Dictionary
Definition
dys-
pref.
1. Abnormal: dysplasia.
2.
a. Impaired: dysgraphia.
b. Difficult: dysphonia.
3. Bad: dyslogistic.
[Latin dys-, bad, from Greek dus-; see dus- in Indo-European roots.]
The American Heritage® Dictionary of the English Language, Fourth Edition copyright ©2000 by Houghton Mifflin Company. Updated in 2009. Published by Houghton Mifflin Company. All rights reserved.
.










Subscribe to RogueMedic.com