Why are more medical directors abandoning the mythology of their ancestors?
Because it has become almost impossible to ignore the absence of evidence of any improved outcomes and the abundant evidence of harm.
Today, in Kansas, Johnson County Med-Act threw a bucket of water on their Long Spine Board Witchcraft and Kansas was not hit by a tornado. Kansas is only being hit with snow.
But there must be some good reason to use backboards!
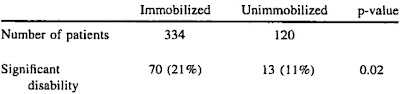
The backboard has been a component of field spinal immobilization despite lack of efficacy evidence.[1]
When there is no evidence of benefit, then it is not an insult to call a treatment witchcraft, dogma, alternative medicine,
Other than historical dogma and institutional EMS culture we can find no evidence-based reason to continue to use the Long Spine board as it currently exists in practice today. The evidence that does exist regarding the Long Spine board is overwhelmingly negative.[2]
There must have been a time, in the beginning, when we could have said – no. But somehow we missed it. Well, we’ll know better next time. – Tom Stoppard
Will we know better next time? Our history does not give us reason to be optimistic about our ability to avoid this error.
We should have said, No.
We should have insisted on evidence.
The history of medicine is full of things that seemed like a good idea at the time.
Seemed like a good idea at the time is just the slightly more respectable form of conbining alcohol, a dangerous idea, and Watch this!
Science is a way of trying not to fool yourself. The first principle is that you must not fool yourself, and you are the easiest person to fool. – Richard Feynman.
We never seem to tire of fooling ourselves.
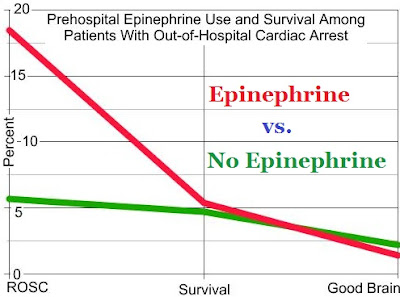
Why am I so critical of tPA for acute ischemic stroke, backboards for potential spinal injuries, furosemide for acute heart failure, ventilations for cardiac arrest, all drugs for cardiac arrest, . . . ?
Because all of these treatments have become standards of care, even though they have not been adequately studied.

Original picture image credit of tPA alternative medicine pusher Dr. Patrick Lyden.
We fool ourselves and harm our patients.
If you disagree, provide some evidence of any of these treatments producing improved outcomes that matter.
We should assume every treatment is harmful, until there is valid evidence that the treatment is safe and effective.
Just like blood-letting and every other superstition-based treatment.
The ambulance stretcher is in effect a padded backboard and, in combination with a cervical collar and straps to secure the patient in a supine position, provides appropriate spinal protection for patients with spinal injury.[1]
Why not just leave out the harmful device that cannot be demonstrated to improve outcomes and cannot even be demonstrated to be safe?
But someone will sue and everyone will lose everything!
Everyone’s got a mortgage to pay. [inner monologue] The Yuppie Nuremberg defense.[3]
It is the EMS Nuremberg Defense when we do it.
it may be common or customary for EMS providers to use a long spine board or collar, decisions of standard of care and negligence are not based on what is the best, reasonable care, not on what is usually done.66 [4]
This witch is only mostly dead, but we can’t stop now.
To read more on the topic –
For You Disciples of Spinal Immobilization…
… Bryan Bledsoe debunks your religion in the August issue of EMS World Magazine. And in that same issue, I take a dump on your altar. Our karma ran over your dogma.
August 1, 2013
by Kelly Grayson
A Day in the Life of an Ambulance Driver
Article
The Evidence Against Backboards – What does the spinal science say?
Bryan E. Bledsoe, DO, FACEP, FAAEM
August 1, 2013
EMS World
Article
Why We Need to Rethink C-Spine Immobilization
By Karl A. Sporer, MD, FACEP, FACP
Created: November 1, 2012
EMS World
Article
In order to protect the c-spine, should we stop helping?
Mill Hill Ave Command
Saturday, December 15, 2012
December 15, 2012
Article
Another Nail in the Board
StreetWatch: Notes of a Paramedic
January 17, 2013
Peter Canning
Article
Does Spinal Immobilization Help Patients? – Who needs c-spine clearance?
Steven “Kelly” Grayson, NREMT-P, CCEMT-P AND William E. “Gene” Gandy, JD, LP
August 1, 2013
EMS World
Article
A Change of the Dogma – If spinal immobilization helps only one . . .
Sun, 15 Jan 2012
Rogue Medic
Article
C-Spine Death Knell with Rogue Medic
Tue, 22 Jan 2013
Rogue Medic
Article
Plastic Snake Oil – EMS Spinal Immobilization
February 24, 2014
Life Under the lights
Article
Some podcasts –
A Change of the Dogma: If it helps only one? Episode 36
First Few Moments
January 12th, 2012
Dr. Laurie Romig, Russell Stine, Bob Lutz, Kyle David Bates, Kelly Grayson, and me.
Podcast
C-Spine Death Knell with Rogue Medic.
John Broyles and me.
January 19, 2013
1-Union-801
Podcast
Immobilization or not that is the question – EMS Garage Episode 156
Chris Montera, Scott Keir, Dr. Dave Ross, Sam Bradley, Patrick Lickiss, and me.
Feb. 24, 2012
EMS Garage
Podcast
And the video that only makes sense if you work in EMS –
–
Footnotes:
–
[1] EMS Spinal Precautions and the Use of the Long Backboard – Resource Document to the Position Statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma.
White Iv CC, Domeier RM, Millin MG; and the Standards and Clinical Practice Committee, National Association of EMS Physicians.
Prehosp Emerg Care. 2014 Feb 21. [Epub ahead of print]
PMID: 24559236 [PubMed – as supplied by publisher]
–
[2] Johnson County EMS System Spinal Restriction Protocol 2014
Ryan C. Jacobsen MD, EMT-P, Johnson County EMS System Medical Director
Jacob Ruthsrom MD, Deputy EMS Medical Director
Theodore Barnett MD, Chair, Johnson County Medical Society EMS Physicians Committee
Johnson County EMS System Spinal Restriction Protocol 2014 in PDF format.
–
[3] Thank You for Smoking
Movie, based on the book by Christopher Buckley
Wikiquote
Quote page
–
[4] Board to Death – The state of prehospital spinal injury care in 2013
Rommie L. Duckworth, LP
Created: July 15, 2013
EMS World
Article
.






Subscribe to RogueMedic.com