
Another Normal Sinus Rhythm post this week. After this week we should be switching to every other week. 🙂
This week, again, there is no theme? Or is it education? In which case I am a bit off topic. Read the rest of the NSR Blog posts at NSR Week 15?
From Respiratory Therapy 101: Just Keep Breathing comes this not-so-shocking description of apparent misbehavior by a doctor – What?:
I was reading a patient’s H&P the other day when I came across the following gem from one of our pulmonologists, who has a history of ordering thousands of dollars of useless therapy for no reason:
“There is no clinically significant bronchodilator response, which does not preclude the use of bronchodilator therapy.“
…Huh? Somebody explain this to me. I’d love to know why “no clinically significant bronchodilator response” does not preclude the use of said bronchodilators. If they don’t work, why are we giving them? Would you give someone Morphine for a staph infection? No, you wouldn’t, because it doesn’t work. So why would you give this patient, who has a repeatable PFT result showing zero response to bronchodilators, a bronchodilator?
This is why healthcare costs so much. Seriously.
This is part of the problem with poor medical care as well as other badly performed jobs. People equate doing something with making things better. Doing something may not be doing something valuable. Doing something may be doing something harmful. Here the doctor states that there is no apparent benefit from giving the bronchodilator to the patient.
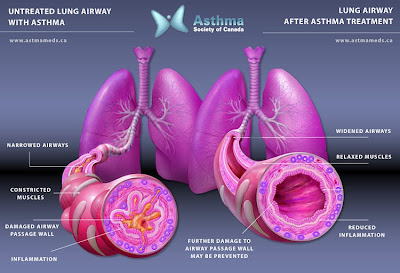
Bronchodilator – beta stimulant used to try to get the bronchial smooth muscles to relax, assuming that brochoconstriction is at least a part of the reason for the patient’s condition. Here is an image from asthmameds.ca/. If you click on the image it will take you to a page about asthma. Click on the image on the left (looks like the image below) and this will open in full size.
Imagine trying to breathe through the airway on the left. This is why so many people die from asthma. Most asthma does not get this bad, but when it does it is life threatening/life ending. If you don’t have any experience with this kind of breathing problem, try breathing through a big straw. A really big straw. The kind that is appropriate for thick milkshakes. Pinch your nose and breathe just through the straw for a while.
If that is comfortable, switch to a normal size of straw and do the same.
If that is comfortable switch to a swizzle stick size or a 14 gauge catheter (without the needle in it).
This restriction of the amount of air coming into the lungs is only a part of the problem with asthma. Mucus blocking these restricted airways complicates things even more.
The bronchodilator is given to the patient to change the condition of the airway, but not when it is already looking like the right side of the image, when the patient does not feel that their breathing is impaired. There are long acting bronchodilators that are taken on a regular basis as preventive therapy. There are times when taking a bronchodilator may help prevent bronchoconstriction (such as before exercise). The pulmonologist did not write anything about treating symptoms.
From the label for Xopenex, a commonly used bronchodilator. It is a type of albuterol that is supposed to be gentler on the body than the regular albuterol. Here is the complete listing of indications:
INDICATIONS AND USAGE:
Xopenex (levalbuterol HCl) Inhalation Solution is indicated for the treatment or prevention of bronchospasm in adults, adolescents, and children 6 years of age and older with reversible obstructive airway disease.[1]
The pulmonologist did not mention anything about prevention in the note. So, as long as the drug is harmless, there should be no problem with this use – other than the requirement for staff and medicine and cost. But why would anyone think about these things in health care?
Is the drug harmless?
Back to the Xopenex label (Warnings and Precautions):
WARNINGS:
- Paradoxical Bronchospasm: Like other inhaled beta-adrenergic agonists, Xopenex Inhalation Solution can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs, Xopenex Inhalation Solution should be discontinued immediately and alternative therapy instituted. It should be recognized that paradoxical bronchospasm, when associated with inhaled formulations, frequently occurs with the first use of a new canister or vial.
- Deterioration of Asthma: Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. If the patient needs more doses of Xopenex Inhalation Solution than usual, this may be a marker of destabilization of asthma and requires reevaluation of the patient and treatment regimen, giving special consideration to the possible need for anti-inflammatory treatment, e.g., corticosteroids.
- Use of Anti-Inflammatory Agents: The use of beta-adrenergic agonist bronchodilators alone may not be adequate to control asthma in many patients. Early consideration should be given to adding anti-inflammatory agents, e.g., corticosteroids, to the therapeutic regimen.
- Cardiovascular Effects: Xopenex Inhalation Solution, like all other beta-adrenergic agonists, can produce a clinically significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, and/or symptoms. Although such effects are uncommon after administration of Xopenex Inhalation Solution at recommended doses, if they occur, the drug may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Therefore, Xopenex Inhalation Solution, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
- Do Not Exceed Recommended Dose: Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs in patients with asthma. The exact cause of death is unknown, but cardiac arrest following an unexpected development of a severe acute asthmatic crisis and subsequent hypoxia is suspected.
- Immediate Hypersensitivity Reactions: Immediate hypersensitivity reactions may occur after administration of racemic albuterol, as demonstrated by rare cases of urticaria, angioedema, rash, bronchospasm, anaphylaxis, and oropharyngeal edema. The potential for hypersensitivity must be considered in the clinical evaluation of patients who experience immediate hypersensitivity reactions while receiving Xopenex Inhalation Solution.[2]
Levalbuterol HCl, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, hypertension, and cardiac arrhythmias; in patients with convulsive disorders, hyperthyroidism, or diabetes mellitus; and in patients who are unusually responsive to sympathomimetic amines. Clinically significant changes in systolic and diastolic blood pressure have been seen in individual patients and could be expected to occur in some patients after the use of any beta-adrenergic bronchodilator.
Large doses of intravenous racemic albuterol have been reported to aggravate preexisting diabetes mellitus and ketoacidosis. As with other beta-adrenergic agonist medications, levalbuterol may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease is usually transient, not requiring supplementation.[3]
like all other beta-adrenergic agonists, can produce a clinically significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, and/or symptoms.[4]
The advice to people who make this mistake in EMS is –
Don’t just do something.
Stand there.
We are supposed to provide needed care. Giving drugs, just because we can, or just because we feel the need to do something, is a bad idea.
I spend more time holding hands than pushing drugs.
Should I be more like the pulmonologist and throw drugs at the patient, while throwing caution to the wind? This is what I perceive the pulmonologist to be doing. Am I wrong? He wrote –
There is no clinically significant bronchodilator response, which does not preclude the use of bronchodilator therapy.
Is there a reason, other than clinically significant response (bronchodilator response in this case), to give a patient a treatment?
If no response is anticipated, no treatment should be given. Medicine is not for the purpose of giving unnecessary treatments. One of the reasons for research is to eliminate treatments that are ineffective and/or harmful.
Treatment purely for the sake of treatment is bad medicine.
The delivery of good medical care is to do as much nothing as possible.[5]
Footnotes:
^ 1 xopenex (levalbuterol hydrochloride) inhalant
[Sepracor Inc.]
FDA label from DailyMed
^ 2 xopenex (levalbuterol hydrochloride) inhalant
[Sepracor Inc.]
FDA label from DailyMed
^ 3 xopenex (levalbuterol hydrochloride) inhalant
[Sepracor Inc.]
FDA label from DailyMed
^ 4 xopenex (levalbuterol hydrochloride) inhalant
[Sepracor Inc.]
FDA label from DailyMed
^ 5 House of God
by Samuel Shem
Laws of the House of God from Wikipedia
.


Scourgeons often say: “The key to being a good surgeon is knowing when NOT to operate”.The same should be applied to all practices.
Allow me to interject myself( a phrase I have uttered none too infrequently in the past) into the fray. Without reading the Pulmonologist’s entire report and the complete results of the PFT it is impossible to know what he was thinking. It is not exactly mental gymnastics to entertain the thought of there being a situation where medications showed little physiological response BUT would be indicated during certain situations!As I sit here (sans hangover) if I were to take 2 acetaminophen, say, you would predict I would also show “no clinically significant response”. HOWEVER should I actively have a headache, or fever, or a little pain- well then the use of the medication may indeed be warranted. Again, you would need to see the entire report of the PFT. Was there a Methacholine challenge done? What is the patient’s FEV1/FVC? Does the patient have exercise-induced asthma? My point is: it is easy to jump to conclusions when not all of the data is in hand. (perhaps another post-inspiring point!)Rogue, I agree that the overriding mantra in medicine should not be to “Do Something”; rather “Do Something Meaningful” Many times Meaningful HCL lies outside of the medicine bag! But let’s not jump to conclusions and make rash judgments without all of the facts.**Congress excluded
ParaCynic,I think that works best for the most risky non-medical jobs, too. Foe example, nuclear weapons launch control officer. That’s just a hunch. 🙂
I was described by a colleague as a “non-interventional paramedic.” It was the rare patient who received ALS treatment in my ambulance, and even then some of them got an IV because it was marginally indicated and I knew the wrath of the ED staff if I delivered the patient without what they would consider “appropriate” interventions.I’ve taken that “wait-and-see” attitude into my organ donor management field as well…I’ll get calls from my staff or hospital staff asking what to do when a donor’s BP is “patent pending over 150 (Shem, House of God). Usually the answer is “let it go for now” and the problem resolves itself. Medical personnel should intervene when necessary, of course, but should also consider how “necessary” that intervention is, and whether it’s likely to make a clinical difference in patient outcomes (including patient comfort).
Vince,I am working on a reply. Maybe next time I will schedule one of these posts for when you do have a hangover. 🙂
Try most days that end in “Y” ;-)Your working on a reply reminds me of Fermat’s infamous quote: “I have discovered a truly marvelous proof of this, which this margin is too narrow to contain.” ;-)Another full-fledged post-in-reply? I can’t wait!
PJ Geraghty,That is precisely the point.I shall try to combine my reply to you and to Vince into one post.
Vince,Sadly, I suspect my reply will be much more marginal than Fermat’s. OTOH, the effect may be more substantial than those of the pulmonologist.I will try not to use too much from Bluff your way in Fermat’s Last Theorem.:-)
You have a very powerful mind that can make anything happen as long as you keep yourself centered.
I’ve always been a believer in medical minimalism. Sometimes the best thing we can do is to do as little as we can.
keepbreathing said… “I’ve always been a believer in medical minimalism. Sometimes the best thing we can do is to do as little as we can.”This is something that people only seem to learn by experience. Although some do practice the stare of life initially, they may deteriorate into actively harming the patient when they get over their shock. Not good for the patient.
I am only a patient, but have had a very bad experience with Xopenex, and a resp doc. 15 years ago I had a breathing test within a chamber and then they gave me albuterol to see if it helped. Rated at 50% before albuterol. I told doc that albuterol made my asthma worse but they said go ahead. After test my breathing was down to 43% and asthma attack had begun.Doc told me to never take Albuterol again, I told him I didn't want to, he made me, he said; "make the doctor listen".Jump ahead to earlier this month, after all this time of having no prescription meds, especially corts, I hear that Primatene inhalers are about to end, only thing that has worked for me in 53 years. So I go to specialist again, similar test without being in a box, first test I find I have increased to 60%, then doc wants to try Xopenex, had tried a sample last year, made asthma worse, told doc, but he insisted that the vaporizing machine would be safer and had me inhaling that stuff for half an hour. My throat went numb, then redid the test and surprise no improvement above 60%, what I expected, but the doc couldn't accept the results and went on about needing to get me on corts, which had almost killed me in the past.Went home after test, began feeling anxiety, then anger.Then I went into paralysis and started having hallucinations. Thought the walls were aglow with fire and maybe because of the smoke couldn't move, made little sense but was trying to come to grips with the experience.This paralysis lasted some 12 hours and at some point voices were telling me to give up because I was already dead. Next day I had fears I was repeatedly falling back into paralysis. Now I refuse to see another doctor about this, my most lifethreatening problem, because doctors will not listen to patients. when Primatene inhalers are gone, I will likely die, the Primatene tablets are too strong and effect my entire body, especially my heart, the mist gets the medicine straight to my lungs, but that will be gone.
We all have identified that we do thousands of unnecessary bronchodilator therapy be Albuterol nebs, mdi through the vent, combivent through the vent. Txs. for chf and pneumonia. What do we need to do about it? Because I am burned out. We need to be weaning our vent patients, not performing useless, not indicated txs.