Cartoon credit.[1]
–
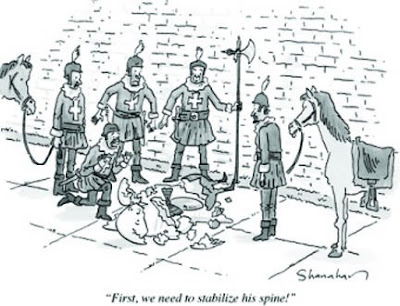
When even the New Yorker is pointing out how ridiculous our obsession with spinal immobilization can be, then maybe it is time for EMS to re-evaluate this placebo.
–
There is still only one large study that looked at outcomes from spinal immobilization –
The difference in neurologic disability between immobilized patients in the United States and unimmobilized patients in Malaysia was statistically significant. It may be that immobilization increases the risk of neurologic injury secondary to tissue hypoxia, perhaps by delaying resuscitation or perhaps the benefit of immobilization is so small that it is unmeasurable given our sample size.[2]
–
How many people end up as quadriplegics because we use spinal immobilization on them?
How many people die, or end up with permanent brain damage, because we place more importance on spinal immobilization than on airway management?
If the airway is difficult to manage, the last thing we will do is remove the sacred cervical stabilization to allow for adequate airway management.
–
Also see –
Allow Me To Manipulate.. I Mean Immobilize Your Spine – Part I
–
Footnotes:
–
[1] “First, we need to stabilize his spine!”
(All the king’s men attempt to save a shattered Humpty Dumpty.)
Published in The New Yorker 12/22/2008
by Danny Shanahan
Link to cartoon
–
[2] Out-of-hospital spinal immobilization: its effect on neurologic injury.
Hauswald M, Ong G, Tandberg D, Omar Z.
Acad Emerg Med. 1998 Mar;5(3):214-9.
PMID: 9523928 [PubMed – indexed for MEDLINE]
.


Evil backboard.
I used a demo vacuum board a little while back. Not a solve all answer to backboarding prayers but I was very pleased with the comfort and level of padding it provided.
One of the more concerning points for me was getting the patient ONTO the vacuum board. Once on though, not bad.
We also tried strapping the vaccum board to a regular rigid board and it provided what I thought to be a very nice “package”. I myself was placed into the device and I personally found it to be, dare I say it- Comfortable.
Im not great at picking out good studies yet but here is one that may be relevent.
http://www.neann.com/vimstudies.htm
Chris,
It isn’t the backboard.
It is the application.
There are many possibilities, but the origin of backboarding is supposed to be as an extrication device only.
Apparently, some rocket scientist decided – “If it can be used for extrication, then it must be used for transportation.”
We seem to look for ways tgo make patients as uncomfortable as possible. The more the patient has to endure to receive treatment, the greater the placebo effect we can produce.
“They wouldn’t have caused me so much pain, unless it was good for me!”
Distinctions between a career in EMS and a career as a sadist are probably not that great – except for the pay.
I will have to take a look at these, but since they all compare the vacuum splint with backboarding, they will not give us any idea of what benefit there might be compared to no immobilization, or to loose motion restriction, or if there is any harm compared to these.
.
It’s kinda like gun control: it’s what you do instead of something. I suspect this will be like the argument over epi in arrest: you’re probably right about the effects of it, but no one wants the liability of a study.
chiefjaybob,
There is no evidence that doing something just to be doing something (backboarding) is not harmful.
Usually, when we are doing something just to be doing something, we find out that what we are doing is harmful.
We may find out that epinephrine is useful in some cardiac arrests, but using it for everyone refractory to defibrillation, or everyone with asystole/PEA (Pulseless Electrical Activity) leads to a lot of inappropriate use. Inappropriate use will cause harm.
The liability issue seems to be one of the lack of good expert witnesses and the willingness of some expert witnesses to claim that they know that not immobilization would be harmful. It is a fraud to distort the lack of evidence of benefit into something they claim supports backboarding.
.
For me, the backboard was always a palette upon which I applied whatever was on hand; pillows, blankets, duct tape if I had to, etc. to place the patient in the most stable position possible in preparation for movement. Of course, depending on the circumstances, it could be the gurney, “Scoop” stretcher or even stair chair. If the tool I was handed was not appropriate to support stability and comfort for transport, then it wasn’t a tool.
The backboard is one of many tools we have available for our use. It is only one way to move a patient from here to there. How that is done is determined by the injury and the patient’s response to it.
firetender,
We should do everything we can to improve the comfort of our patients. Perhaps the best way is to remove the board.
If the tool is appropriate to move the patient to the ambulance, but not appropriate to transport the patient the rest of the way to the hospital, then the tool doesn’t work?
In the previous sentence, you mentioned using the stair chair. Are you suggesting that you transported patients to the hospital in the stair chair?
Are you claiming that the stair chair is not an appropriate tool, unless we can transport the patient to the hospital in the stair chair?
Are you claiming that a tool must be all things at all times, or it is not an effective tool?
We use tools for the specific indications where they are most appropriate, other than that we use a different tool. That does not mean that the original tool is not a
goodtool.A backboard is one of many tools. We have determined that it should be used for something it is not good at and we use our ignorance to justify this.
We could study the benefits and harms of using a backboard for spinal motion restriction, but we choose ignorance over knowledge.
.
Hey,
EMT-B from New Zealand here. Lovin’ the blog.
At the ED I used to take patients to (having just moved cities) it was fairly comon practice to put a collar on a patient before unloading at ED, because the first question we would be asked was “Why is/he not collared?”
This always seemed a stupid practice to me, and it’s a nice change to see some evidence to back up what I always felt.
As a side note, when you post about intubation, do you mean with or without the use of drugs (namely, RSI – rapid sequence intubation) for sedation? Here, we are only just starting in a trial operational use of pre-hospital RSI. Currently the most an Intensive Care Para can do is squirt in some midazolam if they’re struggling too much as it were (though, I guess if they are struggling about that much, they probably don’t need a ‘tube, Right?)
Thanks!
Sam,
Thank you.
That is a bit different. Using a collar is supposed to provide a reminder to the patient to not turn the neck.
Unfortunately, the collars we use in EMS are different from the soft collars used in the hospital. A Philadelphia collar seems to be most commonly used. It seems that the collars we use are designed more for restraint, than reminder.
Restraint may not be a good idea with a patient with a spinal injury.
Physical restraint magnifies the force applied to an unstable fracture.
We should probably use a collar on scene, but not the kind currently used in EMS. Our practice seems to be designed around the idea that the more uncomfortable it is, the better it is for the patient.
I usually will specify that I mean RSI, when I am specifically addressing RSI (real RSI – including a paralytic, an analgesic, and a sedative). There are many significant advantages to using RSI, but there is also increased risk.
Using just midazolam for intubation has not done well in research on intubation.
Without midazolam, the success rate is 91.5%.
With midazolam, the success rate is 62.5%.
This is not a simple comparison of success rates.
Midazolam is only used in this system for those patients who might have a gag reflex, or otherwise be combative. These are expected to be the most difficult tubes, as opposed to the dead patients who make up most intubations. Would things have been better with higher doses of midazolam? Maybe, but this includes trauma patients who may only still be alive due to vasoconstriction. High doses of midazolam would be a bad idea. Even standard doses may be much too much.
Also note that 43.1% of the failed intubations where midazolam was not used, met protocol criteria for use of midazolam. Would that have improved the overall success rate? Would they have improved both the midazolam success rate and the no midazolam success rate? By removing some of the failures from no midazolam group, the success rate would have gone up, but some of the successes would also be removed.
We would not know which intubations would be the failures and which would be the successes. Some of the successful intubations would also qualify for use of the midazolam protocol.
A more interesting consideration is to compare the midazolam intubations here with the RSI (real RSI – including a paralytic, an analgesic, and a sedative) success rates elsewhere.
Places that use RSI should not tolerate a 62.5% success rate. That is about 30% too low.
Is it the midazolam that is the problem? Is it the dose of midazolam that is the problem? Is it a lack of familiarity with midazolam? Is it a lack of skill? Is it some combination of these?
We do not know, but midazolam, as used in this protocol, does not appear to be the solution to intubation of awake patients.
.
So, entirely in theory, what would be the highest GCS you would attempt to ‘tube someone (without drugs)?
Always difficult to change dogma.
Especially in the face of “expert” recommendations.
This is a more recent consensus “expert” recommendation in our neck of the woods : http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3143405/?tool=pubmed
They take a middle road, recommending judicious pre-hospital clearance, which is good : but still insist on immobilisation for those you can’t clear, implying that it NECESSARILY has value if there is a fracture… which contradicts other studies on whether C collars help or not.
This comic is the best thing ever.