.jpg)
Also posted over at Paramedicine 101 (now at EMS Blogs) and at Research Blogging. Go check out the excellent material at these sites.
–
Continuing from Part I, Part II, and Part III.
After assessing what it is that the abdominal pain patients want/expect from a visit to the ED (Emergency Department), how many X-rays it takes to deliver the same radiation as an abdominal CT (Computed Tomographic imaging), whether CTs increase the lifetime risk of cancer, and how many abdominal CTs equal some sort of measure of the radiation exposure of Hiroshima survivors, the authors conclude that people do not understand the risks of radiation.[1] This study is followed by an excellent editorial.
–
The easy conclusion from these findings is, unsurprisingly, that patients are ill informed, and thus efforts to improve their education and awareness should help to mitigate the overuse of imaging and its consequent risks.[2]
Dr. Wears does not discuss the validity of assuming that there is only one right answer to the questions asked. There is also a podcast discussing this study and discussing the editorial, but the podcast is similarly missing the problem with the study taking for granted that there is a single right answer to the study’s questions.[3]
–
First, the “rational person” assumption holds that, given correct information, people should arrive at consistent choices about alternatives (eg, to image or not) based on the net expectation of probabilities and outcomes.2[2]
If we make rational decisions, why do so many of us smoke?
If we make rational decisions, why do so many of us eat to the point of obesity?
If we make rational decisions, why do so many of us spend so much time watching reality TV?
Dr. Wears cites some of the studies that show that we do not make rational decisions. To insist that we make rational decisions is also irrational. Isolated examples of decisions that appear rational do not mean that a person makes rational decisions any more than a stopped clock being right twice a day means that the stopped clock keeps accurate time.
The authors provide excellent examples of irrationality in one question they present.

Click on images to make them larger.
–
How a multiple choice question is presented will affect way the answers are chosen.
Why is there no choice for I don’t know?
For most people not familiar with X-rays and CTs, the only honest and rational answer is I don’t know.
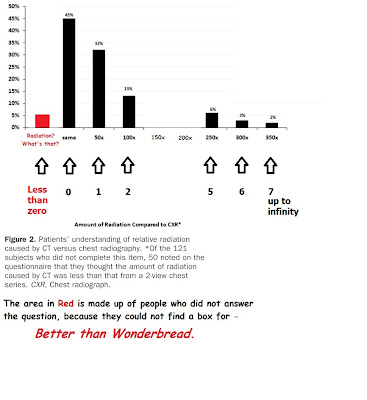
When graphing the results, we can further distort the results by making the distances between numbers completely arbitrary. Why present the choices as the Same radiation (the same, or zero difference is 50 x 0), 50 times more (greater by a factor of 50 x 1), 100 times more (greater by a factor of 50 x 2), 250 times more (greater by a factor of 50 x 5), 300 times more (greater by a factor of 50 x 6), and Over 350 times more (greater by a factor of 50 x at least 7).
–
–
Why blur the distinction between 100 times and 250 times? When the numbers become blurred, the numbers lose their meaning. When there is no difference in meaning between one number and a number 2 1/2 times as large, are we providing information or are we providing confusion?
We seem to most insist on stripping information of its meaning when we create multiple choice tests. Correct answers become a simple matter of memorization separated from understanding. This is one way to create the protocol monkey – the automaton, whom we claim is rendered harmless by being prevented from thinking. This desire to prevent the use of judgment may be the ultimate irrational decision.
If the difference between 100 and 250 is the same as the difference between 250 and 300, how do we expect anyone to notice differences in dosages? 100 mg – 200 mg – 300 mg – what’s the difference? With memorized answers, the only difference is whether it is graded as correct. With real patients, the differences can be fatal.
We memorize our way to recklessness.
We do not memorize our way to safety.
–
Previous literature estimates the radiation dose for an abdomen-pelvis CT to be equivalent to 100 to 250 2-view chest series.2,10-12 For the purpose of this investigation, we used the conservative estimate of 1 abdomen-pelvis CT = 100 2-view chest radiographs.[1]
I agree with their choice to use the more conservative number, but what this still does not do is put this in a context that helps people to understand. Without understanding something about the radiation exposure of an X-ray, this is an unknown. 10 times an unknown – 100 times an unknown – 1,000 times an unknown – what’s the difference?
Presenting misleading information to medically naive people and proclaiming Eureka! is misleading. We are not finding anything. We are presenting a spectacle, although not as much of one as Archimedes did running naked through the streets (assuming the legend to be true).
–
The second assumption is that the problem is “out there” in patients, not “in here” in physicians. This might be viewed as a form of the psychologist’s fallacy,3 the idea that although patients’ preferences might suffer from irrationality, ignorance, or irrelevant considerations, ours (physicians’) do not.[2]
An excellent point that should be extended to researchers.
How much of the problem is in the study design?
What are we measuring?
If the purpose of controlled trials is to examine things objectively, why use a study that seems to depend insist on subjectivity?
–
I will write more about Dr. Wears editorial later, because it covers a lot of important material on making decisions.
–
Footnotes:
–
[1] Patient perceptions of computed tomographic imaging and their understanding of radiation risk and exposure.
Baumann BM, Chen EH, Mills AM, Glaspey L, Thompson NM, Jones MK, Farner MC.
Ann Emerg Med. 2011 Jul;58(1):1-7.e2. Epub 2010 Dec 13.
PMID: 21146900 [PubMed – indexed for MEDLINE]
Free Full Text from Annals of Emergency Medicine with links to Free Full Text PDF Download
–
[2] Risk, radiation, and rationality.
Wears RL.
Ann Emerg Med. 2011 Jul;58(1):9-11. Epub 2011 Apr 2. No abstract available.
PMID: 21459481 [PubMed – indexed for MEDLINE]
–
[3] What patients understand about radiation exposure from CTs
David H. Newman, MD, and Ashley Shreve (spelling?)
Annals of Emergency Medicine podcast page
2011 July
Free Podcast in MP3 format
Annals of Emergency Medicine provides a podcast that summarizes the articles published that month. This is an excellent resource. The full July 2011 podcast is – Free Full Podcast in MP3 format. The full archives of Annals of Emergency Medicine podcasts is – Page with links to podcast segments and full month podcasts.
–
Baumann BM, Chen EH, Mills AM, Glaspey L, Thompson NM, Jones MK, & Farner MC (2011). Patient perceptions of computed tomographic imaging and their understanding of radiation risk and exposure. Annals of emergency medicine, 58 (1), 1-700 PMID: 21146900
–
Wears RL (2011). Risk, radiation, and rationality. Annals of emergency medicine, 58 (1), 9-11 PMID: 21459481
.


I just have a squishy Cultural (Medical) Anthropology degree, but I was taught something about questionnaire design. My Lord, that design stank, for the reasons you gave.
If I know that from one module of one undergrad course in a mostly qualitative social science, and you know this, and Dr Wears knows this, how the Heck did *none* of Baumann et al or their reviewers know this?
I would like to show my thanks to the writer just for bailing me out of this crisis. Just after surfing around throughout the world wide web and coming across strategies that were not pleasant, I figured my entire life was done. Existing without the presence of answers to the issues you’ve sorted out by way of the review is a critical case, as well as the ones which may have in a wrong way affected my career if I had not come across your site. Your actual understanding and kindness in playing with all areas was tremendous. I’m not sure what I would have done if I had not come upon such a stuff like this. It’s possible to at this moment look forward to my future. Thank you so much for the reliable and results-oriented guide. I won’t hesitate to endorse your blog to any individual who would need support on this area.