Do we have to use long spine board immobilization?
The traditional method for moving and transporting trauma patients has been with the patient in a supine position on a backboard to protect the spine. These are the guidelines that are taught presently in standard traumatology courses such as the Advanced Trauma Life Support (ATLS) and Prehospital Trauma Life Support (PHTLS) courses [1-3]. [1]
–
Should we keep placing spinal immobilization comes before airway and circulation?
I know that we are not supposed to, but look at the way spinal immobilization is actually used.
According to international resuscitation guidelines [9,10], the lateral-recovery position should be used when an unconscious patient is breathing to maintain airway patency; it is further stated that “efforts to protect the cervical spine must not jeopardize oxygenation and ventilation” [9]. [1]
–
What alternatives are there to spinal immobilization on a long spine board?
PHTLS Norway has adopted LTP in their educational program (Sindre Mellesmo, personal communication). In addition to being demonstrated in PHTLS courses, LTP is now part of the written protocols in some Norwegian EMS and is described in the Scandinavian recommendations [13]. [1]
–
But nobody is crazy enough to do something that protects the patient, because the lawyers will do all sorts of mean things to us, and to our dogs.
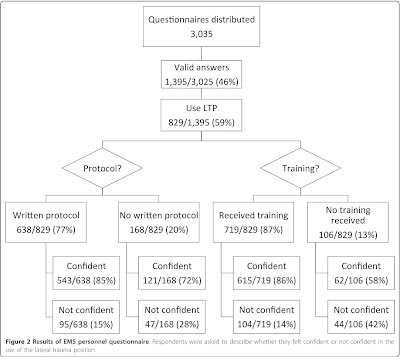
About half of the EMS personnel surveyed answered the survey.
More than half of those EMS personnel do use LTP (Lateral Trauma Position).
–
Click on the images to make them larger.
–
According to the Utstein Formula of Survival [20], medical science, educational efficacy, and local implementation are all necessary factors for survival. In the case of LTP, we have no medical science about the position that would indicate if it indeed is the optimal method for transporting unconscious trauma patients. We have little, if any, knowledge of the right or wrong way to position patients or of the possible dangers of the use of LTP. Educational efficacy and local implementation have, in this case, gone ahead of medical science. [1]
How is that different from spinal immobilization?
There does not appear to be any evidence of increased disability with the use of LTP.
We do need to study methods of transporting patients with potential spinal injuries to find out if any of these methods actually provide any benefit.
To those claiming that it would be unethical to compare spinal immobilization with a no treatment group, this is an acceptable means of spinal immobilization, at least in Norway.
Study long spine board immobilization against Lateral Trauma Position.
Come up with some evidence of benefit or stop using long spine board immobilization.
–
Footnotes:
–
[1] The lateral trauma position: what do we know about it and how do we use it? A cross-sectional survey of all Norwegian emergency medical services.
Fattah S, Ekås GR, Hyldmo PK, Wisborg T.
Scand J Trauma Resusc Emerg Med. 2011 Aug 4;19:45.
PMID: 21816059 [PubMed – in process]
Free Full Text from PubMed Central with links to PDF Download
.



I’d like to see more information.
I’m a little skeptical of this survey.
It suggests that 59% of the respondents use LTP, and that 77% of those have protocols to do so and 89% have had training to do so- yet I’ve never seen it done, and never had it shown to me at all.
It’s possible that where I am is just that “conservative” but it makes me wonder where the survey responses came from.
I’m not saying I disagree with the concept. I don’t know enough about the risk:benefits to have an opinion.
It just surprises me to have such a high percentage claim to do something, and to have protocols and training to do something, that I’ve never seen anyone do, ever.
Lateral position for various medical reasons, I’ve seen. But for trauma? With a collar, and no backboard? Never seen it or even heard it suggested until now.
hilinda,
The study is from Norway. This is being taught as a part of PHTLS in Norway.
The full text of the paper is available at the link in the footnotes.
–
My purpose in writing this is to show that we can change policy. We just need to stop hiding behind the words Standard Of Care.
–
This is just one more reason we need to realize that long spine board immobilization does not need to be a Standard Of Care.
.
to me it sounds like the wrong approach to the right change in standards, airway is was and will always be first priority however i can’t see myself rolling a trauma patient on to a stretcher without a longboard but i can’t see why a compromise can’t be found. to me a combination of back boarding procedures and left lateral position has to be out there.
Anonymous,
We roll trauma patients onto long spine boards, so the rolling is not really different.
The patient should be more stable from sinking into the mattress on the stretcher, at least a little bit. The long spine board does not really do anything more to prevent movement, but the long spine board does increase the discomfort of the patient and increase the amount of straining against the straps and collar. If anything is going to increase the damage of unstable spinal injuries, the long spine board is it.
What kind of compromise is appropriate between what we do, which appears to double the rate of disability from spinal injuries and something that has no apparent history of causing harm?
We should not have implemented long spine board immobilization without some sort of plan to assess outcomes. We assumed that long spine board immobilization would be the best of all possible treatments in the best of all possible worlds.
This was a ridiculous thing for us to assume. Dr. Norman McSwain needs to consider research and alternatives, or someone more interested in what is best for patients needs to be making decisions for PHTLS (PreHospital Trauma Life Support) in the US.
.