What is this and how should we handle it?
A 46-year-old man presented to the otolaryngology clinic with hearing loss and a sensation of fullness in the left ear. The symptoms had started a few days before presentation. He had no other neurologic symptoms.[1]
Do we take anyone else’s assessment for granted?
No, but this is all that we can get in this case.
The patient reported no history of head injury but said that he had been having partial memory blackouts since drinking alcohol at a New Year’s party 5 days earlier.[1]
In vino veritas,[2] so it must be the truth.
Right?
Assume the otolaryngologist, or general practitioner, or somebody, calls for an ambulance.
How do you handle this patient?
Why?
↓
↓
↓
↓
↓
↓
↓
↓
↓
↓
↓
↓
In the hospital, this is the scan of his brain –
White is usually blood on a CT (Computed Tomography) scan of the brain, so this is probably not a good thing, but this is not what we would have known before transport.
How would management, the medical director, and everyone else feel about the way that you handled this?
Would it have made any difference?
–
Footnotes:
–
[1] Battle’s Sign
Kenta Watanabe, M.D., Ph.D., and Wataru Kida, M.D.
N Engl J Med 2012; 367:1135September 20, 2012
Images in clinical medicine
Free Full Text from N Engl J Med
–
[2] In vino veritas
Wikipedia
Article
.

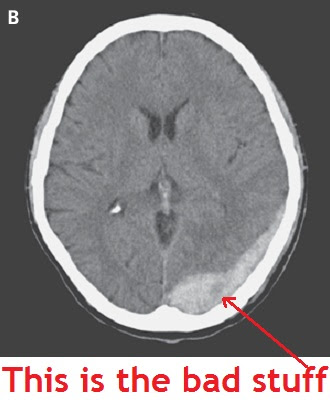


Battle’s Sign, usually being a sign of a skull fracture, and usually associated with underlying brain trauma, specifically intracranial bleeding.
With this patient, monitor vital signs, support the airway, try to minimize unnecessary movement to the head to prevent other trauma (perhaps padding with towels during transport, we all have seen the way our patients’ heads can flop back and forth in a bumpy ambulance), IV access in anticipation of a CT scan, and the most important part would probably be a call ahead to the hospital, ideally one with on-staff neuro, to let them know that this patient should go almost immediately to CT. Monitor BP, be prepared to protect the airway, cardiac monitoring, routine ALS care, and a slow Code 3 to the hospital.
My medical director would probably be upset with me because I would NOT, with all capital letters, subject this patient to full spinal precautions. My system does not allow c-spine clearance in the field and demands immobilization on pretty much anyone who has a “mechanism of injury,” because we are not trusted to assess our patients. Using your information to put together an “assessment” in my head, spinal precautions would offer no benefit and could potentially cause harm with an increase in ICP.
Should be a slow Code 2, minimize stimulation and the easiest ride possible. Lights and sirens don’t save time, and they do make for a bumpier ride.
Based on the information the crew would have, this patient can be triaged to BLS for transport to a neuro-surgical capable hospital. No IV or cardiac monitor needed.
Forgot to mention that my old medical director would have seen “epidural hematoma” on the disposition and “dinged” the medics for turfing the patient to BLS despite fact he was stable and in need of nothing other than transport for evaluation. I imagine most medical directors would act similarly, sadly.