At Life Under the Lights Ckemtp asks, If You Could Have Anything You Wanted… what would it be.
My favorite response was not very aggressive sedation and pain management treatment options – all on standing orders and similarly aggressive IV NTG and CPAP options – also on standing orders. OK, that was my response. My favorite response was from Greg Friese, who blogs at Everyday EMS Tips –
When I was in New York, I had to do a refresher course. Everybody had to do the same things. The guy from New York City, who averaged more than an intubation a week, and the guy from the sticks, who might average an intubation a year.
What kind of EMS system would ignore the differences in experience?
Right?
How about all of them? Maybe that is unfair. Pennsylvania allows medics to decide what courses to take, as long as half of the year’s 18 con ed credits are in the medical/trauma category. That means most of the alphabet soup of merit badges.
Are merit badge courses the only way of demonstrating competence?
Do merit badge courses demonstrate competence?
Certainly not. And. Absolutely not.
I write that as someone who has made a lot of money teaching a lot of these merit badge courses.
–
What does a classroom course tell me about the way someone behaves in a patient’s home?
That may depend on how much imagination I have and on how willing I am to engage in self-deception.
The best place to learn about the competence of the paramedic is probably in the ED (Emergency Department) at the time of transfer of patient care.
Does the treatment given by the paramedic match the patient presentation?
Does the treatment withheld match the patient presentation?
We understand that some patients will have dramatic changes in presentation –
Hypertensive CHF patients after a couple dozen NTG (NiTroGlycerin) and CPAP (Continuous Positive Airway Pressure).
Well sedated patients.
Patients with their severe pain decreased to the comfortable level.
Anaphylaxis patients.
Hypoglycemic patients.
Et cetera.
Medical directors should understand what the normal progression of these diseases is, and recognize when the patients have received appropriately aggressive care and when the patients have not.
Basing competency recertification on a classroom approximation of real patient care is just not appropriate.
–
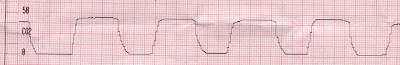
When a patient is in need of a pacemaker, is the pacemaker applied properly? Is the pacemaker actually pacing the heart, or just causing a lot of muscle twitching? Does the paramedic know the difference?
Conversely, if a patient, who should have a pacemaker applied, does not have a pacemaker applied, is there some good reason the paramedic did not apply the pacemaker?
When a patient is taken to a trauma center, does the patient actually have injuries that indicate the patient should be transported to the trauma center?
Conversely, when a patient, who should have been transported to a trauma center, is transported to the local non-trauma center, is there some good reason the paramedic did not transport to the trauma center?
There are many such examples. They require an involved medical director and emergency medicine group interested in good prehospital care/competence.
–
If a paramedic has obtained at least 18 con ed hours each year for 5 years, but cannot tell the difference between a trauma patient and a non-trauma patient, how is the con ed requirement helping?
If a paramedic has obtained at least 18 con ed hours each year for 10 years, but cannot obtain capture with a transcutaneous pacemaker, how is the con ed requirement helping?
If a paramedic has obtained at least 18 con ed hours each year for 15 years, but gives Lasix to patients with pneumonia, how is the con ed requirement helping?
If a paramedic has obtained at least 18 con ed hours each year for 20 years, but needle decompresses a patient’s chest when the patient is talking with him in no apparent distress (at least before the harpooning), how is the con ed requirement helping?
We need to be much better at tailoring our recertification requirements to the needs of the paramedics.
X number of hours in a classroom ≠ competence.
.


.jpg)

Subscribe to RogueMedic.com