In the comments to Comment on ALS is Oxygen, IV, Monitor, and Transport – Part I, there is this from Brandon Oto of EMS Basics.
My apologies for skimming, Rogue. On closer look I see the P waves. I do hold, though, that at certain rates, when atrial activity is obscured as it often is, it can be reasonable to make presumptive rhythm calls based largely on rate, or at least carefully considering it.
I agree that it is reasonable to shock an unstable tachycardia if I cannot identify P waves.
However, I see this as even more reason for a thinking medic.
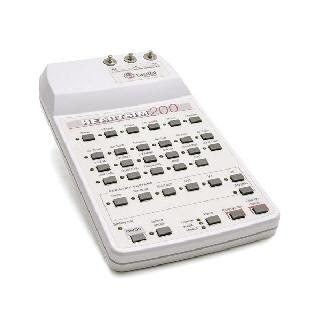
Reading ECGs can be an art form. I have spent a lot of time working on learning to read rhythms while they are moving on the monitor. I think that this is a neglected part of paramedic education. Rhythm generators do have the ability to present rhythms in a testing format.
I press the test button. The rhythm is shown moving across the screen and I have to identify it using the various buttons. I also have to identify any ectopy. While this is not perfect, it allows for a lot of practice. The weird stuff that we may only see on Tom’s blog EMS 12 Lead will be some of what will come up in the testing.
–
–
Looking at unusual rhythms is not important for being able to recognize these unusual rhythms. That is just memorization, which is not the way to get medics to think.
Looking at unusual rhythms is important for learning how to approach rhythm analysis. One of the most important parts of rhythm analysis is getting comfortable with a method that includes all of the essentials.
P Waves?
PR Interval?
P-to-P Interval?
QRS Complex width?
QT Interval?
R-to-R Interval?
Rate?
Axis?
There is no right order for these. Even the search for a PR Interval may be a part of an attempt to determine if what I am looking at are actually P Waves. This is not something that responds well to formulas that can be put into protocols. The important thing is to cover all of these in whatever way works. If I remember things one way, but you use a different order, there is nothing wrong with that.
All of this also requires a thorough understanding of the information that can be obtained from each of these. All of the intervals should be looked at for regularity.
Irregular = Arrhythmia (absence of a normal sinus rhythm or regular sinus rhythm).
Just because something is irregular does not make it unhealthy.
Athletes tend to have a lot of vagal tone, which is healthy. This healthy vagal tone leads to irregularity in the P-to-P Interval. As we breathe in, our heart rate will increase. As we breathe out, heart rate will decrease. With increasing intrathoracic pressure, such as when ventilating a patient by BVM (Bag Valve Mask), blood return to the heart will decrease. This is one of the reasons we keep decreasing the amount of ventilation we provide in cardiac arrest. Eventually, we will eliminate it from the first 5, 10, 15 minutes of CPR, but we have not accepted that, yet.
Anyway, the point of that diversion is to think about what we are doing.
An irregular sinus rhythm may be completely healthy.
A fast sinus rhythm may be completely healthy.
An arrhythmia may not be a sign of an heart problems, but purely a response to pathophysiology. Physiology is just a fancy word for the way the body works. Pathophysiology is a fancy word for the way the body works when something is wrong.
I chose this rhythm strip for one specific reason.
–
–
Very fast, and I thought obvious, P Waves.
Part of the problem with looking at this is the way we are taught.
How many of us are told that faster than 150 is not sinus tachycardia?
Or that faster than the calculated maximum heart rate cannot be sinus tachycardia?
220 minus age = maximum heart rate.
An alternative is 200 minus half of the age = maximum heart rate.
This is nonsense, but if we hear it enough, we may subconsciously apply it to the way we interpret ECGs.
There are P Waves. I thought that the rate was about 220 – the maximum possible calculated heart rate for an infant according to the misinformation formula.
One of the reasons for using this was to get people to ignore this mythological formula. I had not even noticed paid attention to the information that is printed on the strip 50 mm/second. The paper is running through the printer at twice the normal speed of 25 mm/second (1 inch/second). Twice the print speed means that the rhythm is slowed down and spaced out to make it easier to identify things that may be harder to spot at the normal speed. Twice the print speed means that the heart rate is twice as fast as the normal box measurement method would come up with.
This rate is over 400. This is from a dog. I have never seen a human heart beat that quickly, but I have seen close to 300 in human infants.
What would you say if it were ~300? Still could be sinus? How about irreg. irreg. at ~275? How about very wide and regular at 220?
Funny that you should ask about a rate of around 300. The patients I have seen with close to that rate have been infants. Febrile, dehydrated, irritated, and/or in pain infants with sinus tachycardia.
This points out the primary point about sinus tachycardia.
Sinus tachycardia does not get better with cardioversion.
If the rate is so fast that you thing the synchronizer will not get capture, then you should defibrillate shockable rhythms, but sinus tachycardia is not a shockable rhythm.
Sinus tachycardia does not get better with defibrillation.
If judged to be sinus tachycardia, no specific drug treatment is required. Instead, therapy is directed toward identification and treatment of the underlying cause. When cardiac function is poor, cardiac output can be dependent on a rapid heart rate. In such compensatory tachycardias, stroke volume is limited, so “normalizing” the heart rate can be detrimental.[1]
Sinus tachycardia is a symptom of something else. Sinus tachycardia is not a diagnosis.
–
Still could be sinus?
Yes. Absolutely still could be sinus.
How do we determine if a rhythm is sinus?
There are P Waves.
There is a regular PR Interval for the sinus beats.
If there is ectopy, that means a sinus rhythm with _______ ectopic beats, but that is still a sinus rhythm.
P Waves with regular PR Intervals identify a sinus rhythm. Sinus tachycardia is a sinus rhythm.
The rate does not rule out a sinus rhythm.
–
How about irreg. irreg. at ~275?
You are describing something very different from the strip I presented. 🙂
Irregularly irregular should be presumed to be A Fib (Atrial Fibrillation) – until proven otherwise. Why would I assume that something irregularly irregular is a sinus rhythm? Do you have a strip of this A Fib that you expect to be confused for a sinus rhythm? The strip I provided had clear P Waves with a regular PR Interval.
–
How about very wide and regular at 220?
Are there P Waves?
Is there a regular PR Interval for these beats?
The presence of P Waves with an irregular PR Interval would be evidence of V Tach (Ventricular Tachycardia).
An irregular PR Interval would be evidence of dissociation and would probably lead to the conclusion that the rhythm is V Tach.
The wide complex is much less important than the PR Interval in determining if the rhythm is V Tach.
Sinus tachycardia is NOT treated with cardioversion.
–
Sinus rhythm IS treated by treating the cause.
The cause of sinus tachycardia is not a lack of electricity.
–
Footnotes:
–
[1] Sinus Tachycardia
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science
Part 8: Adult Advanced Cardiovascular Life Support
Part 8.3: Management of Symptomatic Bradycardia and Tachycardia
Regular Narrow-Complex Tachycardia
Free Full Text from Circulation with links to Free Full Text PDF
.


In the pediatric population, if the P-waves look a bit off, one should consider an incessant atrial tachycardia or with normal P-waves, inappropriate sinus tachycardia. The interesting part about both of these arrhythmia is that even though pharmacologic intervention is indicated, it likely won’t work!
Christopher,
In the adult population, V Tach is aggressively treated with pharmacologic intervention, even though it is likely that the drugs will not work. 😕
.
Thanks for the response, Rogue! Public shaming, eh? That’ll teach me to skim a strip on the way to work 😀
Okay, here is all that I really meant. In the lack of clear P-wave association, considering the rate becomes a potentially relevant factor to consider in your interpretation. Undoubtedly the “typical” ranges are mutable, and sinus can be as slow as the Nile or as fast as greased lightning, but that just says it’s not a perfect indicator, and nothing is perfect. It’s just one piece of the puzzle.
What I meant by my examples was — supposing I tell you nothing else, but I tell you there’s a rate of 300. Construct a differential based on that alone. Will sinus tach be at the top? Probably not. Probably at the bottom. (There’s a neat strip of 1:1 flutter at 300 I saw recently — baby, of course…)
This isn’t as good of a waysign as finding, or finding the clear lack of, obvious associated P waves! But my whole point is that at certain rates, and in certain rhythms, and in certain situations (i.e. bouncing down the road, or in my case, skimming on my Droid…), P wave associate is not always clear, and that’s why a bigger picture can be helpful.
I’m also not entirely sure whether sinus tachycardia is really something that needs to be “ruled in.” Is this something we need to “catch”? To me, if you’re not certain, ST is more of a diagnosis of exclusion. If things are unclear, you don’t say “welp, just sinus tach” unless you’ve ruled out everything else. And if you screw up and shock it, what’s the worst case? You gave them some unneeded electricity, which is not great, and very embarrassing, but not the end of the world, and now you know. It’ll delay finding and correcting the cause of the tachycardia, but I submit this is a less time-sensitive goal than correcting a life-threatening arrhythmia (i.e. VT).