Continuing with the answer to Where are the Black Box Warnings on These Drugs – I.
There is a black box warning on droperidol for prolonging the QT segment, but there is no black box warning for this commonly used EMS drug (Drug X) that also prolongs the QT segment. Are we supposed to think that Drug X is safer than droperidol?
What is Drug X?
–
Proarrhythmia
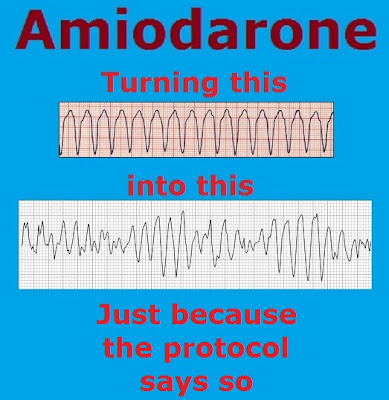
Like all antiarrhythmic agents, amiodarone I.V. may cause a worsening of existing arrhythmias or precipitate a new arrhythmia. Proarrhythmia, primarily torsades de pointes (TdP), has been associated with prolongation by amiodarone I.V. of the QTc interval to 500 ms or greater. Although QTc prolongation occurred frequently in patients receiving amiodarone I.V., torsades de pointes or new-onset VF occurred infrequently (less than 2%). Patients should be monitored for QTc prolongation during infusion with amiodarone I.V. Combination of amiodarone with other antiarrhythmic therapy that prolongs the QTc should be reserved for patients with life-threatening ventricular arrhythmias who are incompletely responsive to a single agent.[1]
Have you ever been warned about the possibility of inducing torsades de pointes or new-onset VF with amiodarone?
What is the incidence of torsades de pointes or new-onset VF with droperidol?
Much much less than 2%.
Although QTc prolongation occurred frequently in patients receiving amiodarone I.V., torsades de pointes or new-onset VF occurred infrequently (less than 2%). Patients should be monitored for QTc prolongation during infusion with amiodarone I.V.
Where is the black box warning for amiodarone for more frequent torsades and VF?
–
–
Maybe you have not seen torsades even with semi-frequent administration of amiodarone.
How many people have seen torsades even with more frequent administration of droperidol?
–
Electrolyte Disturbances
Patients with hypokalemia or hypomagnesemia should have the condition corrected whenever possible before being treated with amiodarone I.V., as these disorders can exaggerate the degree of QTc prolongation and increase the potential for TdP. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or in patients receiving concomitant diuretics.[1]
Have you ever been warned to avoid giving amiodarone to hypokalemic or hypomagnesemic patients?
In EMS, other than guessing based on the patient’s history, how would we know that the patient has hypokalemia or hypomagnesemia?
In the ED (Emergency Department), are magnesium or potassium levels checked before giving amiodarone?
Why does droperidol have a black box warning?
Amiodarone is associated with more frequent torsades and VF than droperidol.
We give out amiodarone more often than banks give political donations.
Why doesn’t amiodarone have a black box warning?
–
Footnotes:
–
[1] AMIODARONE HYDROCHLORIDE injection, solution
[Bedford Laboratories]
FDA label
Label
.


Of mild interest, the FDA just slapped a black-box warning on dronedarone, amiodarone’s troublesome brother. It’s not linked to the actual QT-effects, which I am certain dronedarone shares, just an increase in overall cardiovascular events in patients on the drug for longstanding a-fib. This particular piece of news shouldn’t change our (probably already low) opinion of amiodarone, but it’s a piece of the puzzle showing this class of drugs isn’t benign. But then again, we hopefully already knew that…