.jpg)
Also posted over at Paramedicine 101 (now at EMS Blogs) and at Research Blogging.
–
Go check out the rest of the excellent material at both sites.
Over at 510 Medic, there is an interesting abstract of a new article on treatment of tension pneumothorax. Frequency of Inadequate Needle Decompression in the Prehospital Setting.
CONCLUSIONS: In this study, 26% of patients who received needle thoracostomy in the prehospital setting for a suspected PTX appeared not to have had a PTX originally, nor had 1 induced by the needle thoracostomy. It may be prudent to evaluate such patients with bedside ultrasound instead of automatically converting all needle thoracostomies to tube thoracostomies.[1]
I have not read the full text. I do not have access to this journal. If anyone can send me the full text, I would like to address some of the details, rather than just speculate about them. Late entry – I have received the article. Thank you to Jeff Williams and Jeremy Blanchard. I will write more about the full text later on.
510 Medic makes some important points and asks some good questions. Then 510 Medic asks –
So if we subscribe to the goal of “first do no harm” and those 15 patients didn’t have a pneumothorax induced by the procedure, is their discomfort worth proper treatment for the remaining 42 patients?[2]
I think that there is a more important question.
Should we assume that the presence of a pneumothorax is an indication for needle decompression?
A pneumothorax is not the same as a tension pneumothorax. Even the definition of a tension pneumothorax is not easy to agree on. I tend to treat with opioids what many others would treat with needle decompression. I have not had any of these patients deteriorate, while in my care. They received chest tubes in the trauma center.
Should we assume that the presence of a pneumothorax is an indication for needle decompression?
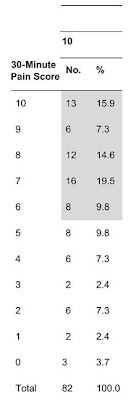
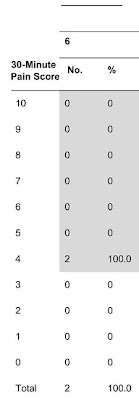
57 patients with a prehospital diagnosis of tension pneumothorax. Yes, EMS does diagnose, but that is a discussion for elsewhere. Yes, these patients were diagnosed by EMS with tension pneumothorax, unless we are suspecting acupuncture, because what other prehospital indication is there for sticking a needle into a patient’s chest?
Out of 57 patients diagnosed with tension pneumothorax, only 42 patients had a pneumothorax.
How many patients had a tension pneumothorax at the time the needle was stuck into the chest wall?
How many of those patients would have been better off if treated with something other than a needle?
How many complications were there from the needle decompression?
Am I wrong to use italics to highlight the word decompression, since so many of the patients did not have anything to decompress?
We rush to perform procedures that we have little experience with. Isn’t this a situation likely to lead to misdiagnosis?
Isn’t the infrequent use of needle decompression for suspected tension pneumothorax likely to lead to operator error?
The actual occurrence of tension pneumothorax appears to be much less frequent than the prehospital diagnosis of tension pneumothorax. Isn’t that an indication of a failure to properly educate medics?
Footnotes:
[1] Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study.
Blaivas M.
J Ultrasound Med. 2010 Sep;29(9):1285-9.
PMID: 20733183 [PubMed – in process]
Free Full Text from J Ultrasound Med.
–
[2] Frequency of Inadequate Needle Decompression in the Prehospital Setting
510 Medic
Article
–
Blaivas M (2010). Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 29 (9), 1285-9 PMID: 20733183
.









Subscribe to RogueMedic.com