.jpg)
Also posted over at Paramedicine 101 (now at EMS Blogs) and at Research Blogging. Go check out the excellent material at these sites.
–
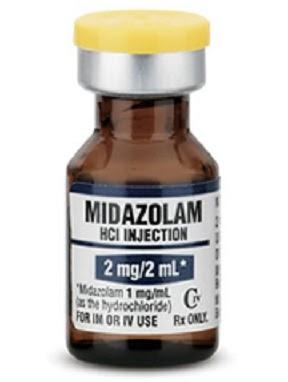
I have already pointed out my disappointment with the references of this large double-blind, randomized, noninferiority trial comparing IM (IntraMuscular) midazolam (Versed) with IV (IntraVenous) lorazepam (Ativan). One of those criticisms appears to be just due to a typographical error. The footnote in the text was 11, but the footnote should have been 1.
The relationships among benzodiazepine dose, respiratory depression, and subsequent need for endotracheal intubation are poorly characterized, but higher doses of benzodiazepines may actually reduce the number of airway interventions. Our data are consistent with the finding that endotracheal intubation is more commonly a sequela of continued seizures than it is an adverse effect of sedation from benzodiazepines.11 [1]
–
Here is some of the information from footnote 1. One interesting aspect of this double-blind study is that there is a placebo group. Patients received 2 mg IV lorazepam, 5 mg IV diazepam (Valium), or IV placebo. Treatment could be repeated one time if seizures continued for more than 4 minutes or if seizures recurred.
Cardiorespiratory complications before arrival at the hospital and at the time of transfer were important secondary outcomes that relate to the safety of out-of-hospital therapy with intravenous benzodiazepines. Despite concern regarding the adverse effects of these agents, we found a trend toward lower rates of out-of-hospital complications (primarily respiratory compromise) in the active-treatment groups than in the placebo group. This suggests that respiratory complications associated with prolonged seizures may be more pronounced than those caused by intravenous lorazepam and diazepam given at relatively low doses.[2]
The doses are low. The lorazepam dose is only half of the 4 mg used in the IV lorazepam vs. IM midazolam study.
The doses of midazolam and lorazepam used in this trial are consistent with the most effective doses for the treatment of status epilepticus that are reported in the literature.9,10 Although these initial doses are higher than the ones used by many EMS systems and emergency physicians, they are the same as those approved for this indication and are in line with those used by epileptologists.[1]
–
Is there added safety from the lower doses?
The epilepsy specialists and the FDA (Food and Drug Administration) do not recommend lower doses.
Were the low doses effective?
–
2 mg midazolam?
Does anyone really expect such a small dose to make a difference?
–
Despite the beneficial outcomes associated with intravenous lorazepam and diazepam, 41 to 57 percent of patients who received active treatment were still in status epilepticus at the time of arrival at the emergency department. These patients were more than twice as likely to require intensive medical care as those whose seizures ended outside the hospital. Differences in the causes of the episodes of status epilepticus are unlikely to account for this difference. These observations, coupled with the favorable risk–benefit profile associated with lorazepam and diazepam in this trial, suggest that higher doses should be studied to define the optimal therapy for patients with out-of-hospital status epilepticus.[2]
An editorial refers to the study just published[1] and to the benzodiazepine vs. placebo study.[2] Describing the complications in the placebo study, the author wrote –
Successful termination was much more common in the two groups that received benzodiazepines (59% with lorazepam, 43% with diazepam, and 21% with placebo). Since respiratory distress was twice as common in the group given placebo as in either of the groups given a benzodiazepine, the best way to avoid the need for intubation is to stop seizure activity.[3]
This presents an interesting conundrum. Doses of benzodiazepines (midazolam, lorazepam, diazepam, . . .) are often limited, due to a fear of causing respiratory complications.
When treating seizures, higher doses of benzodiazepines may actually protect patients from respiratory complications.
With a fatality rate around 10%, seizures are certainly not benign.
Maybe early treatment with high dose benzodiazepines can significantly decrease that fatality rate.
–
Finally, relatively few out-of-hospital interventions have been evaluated in randomized controlled trials,16 and when they have been evaluated carefully, therapies with intuitive appeal have often been found either to lack benefit or to cause harm to patients.17-20 [2]
The irony is that we may be doing the opposite by limiting doses of benzodiazepines to less than what is recommended by the FDA.
What do you think?
–
I have written about this in Intramuscular Midazolam for Seizures – Part I,
Part II,
Part III,
Part IV,
Part V,
Part VI,
Misrepresenting Current Topics in EMS Research from EMS Expo – RAMPART,
and Images from Gathering of Eagles Presentation on RAMPART.
–
Footnotes:
–
[1] Intramuscular versus intravenous therapy for prehospital status epilepticus.
Silbergleit R, Durkalski V, Lowenstein D, Conwit R, Pancioli A, Palesch Y, Barsan W; NETT Investigators.
N Engl J Med. 2012 Feb 16;366(7):591-600.
PMID: 22335736
Free Full Text from N Engl J Med.
–
[2] A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus.
Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S, Gottwald MD, O’Neil N, Neuhaus JM, Segal MR, Lowenstein DH.
N Engl J Med. 2001 Aug 30;345(9):631-7. Erratum in: N Engl J Med 2001 Dec 20;345(25):1860.
PMID: 11547716 [PubMed – indexed for MEDLINE]
Free Full Text from N Engl J Med. with link to PDF Download
–
[3] Intramuscular versus intravenous benzodiazepines for prehospital treatment of status epilepticus.
Hirsch LJ.
N Engl J Med. 2012 Feb 16;366(7):659-60. No abstract available.
PMID: 22335744 [PubMed – in process]
–
Silbergleit, R., Durkalski, V., Lowenstein, D., Conwit, R., Pancioli, A., Palesch, Y., & Barsan, W. (2012). Intramuscular versus Intravenous Therapy for Prehospital Status Epilepticus New England Journal of Medicine, 366 (7), 591-600 DOI: 10.1056/NEJMoa1107494
–
Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S, Gottwald MD, O’Neil N, Neuhaus JM, Segal MR, & Lowenstein DH (2001). A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. The New England journal of medicine, 345 (9), 631-7 PMID: 11547716
–
Hirsch LJ (2012). Intramuscular versus intravenous benzodiazepines for prehospital treatment of status epilepticus. The New England journal of medicine, 366 (7), 659-60 PMID: 22335744
.



















Subscribe to RogueMedic.com